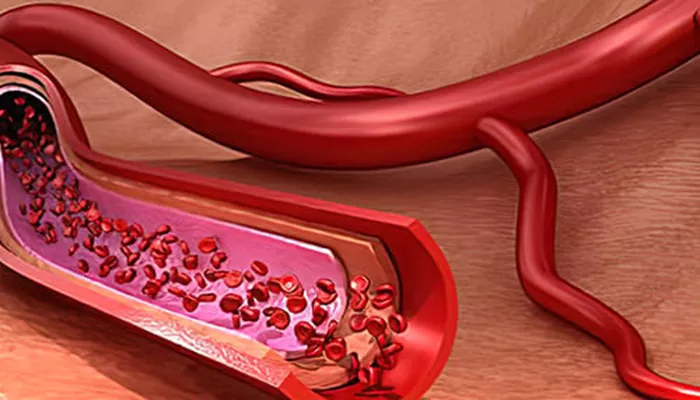
Vasoconstriction is a vital physiological process in which blood vessels narrow due to the tightening of smooth muscles in their walls. This narrowing reduces the diameter of the blood vessels, which in turn decreases blood flow to certain areas of the body. Vasoconstriction plays a key role in regulating blood pressure, controlling blood distribution, and maintaining body temperature.
Understanding Vasoconstriction
The term “vasoconstriction” comes from “vaso,” meaning blood vessel, and “constriction,” meaning narrowing. When the smooth muscle cells in the walls of arteries and arterioles contract, the vessel lumen becomes smaller. This contraction leads to a reduction in blood flow volume and an increase in vascular resistance, which raises blood pressure.
The opposite process is vasodilation, where blood vessels relax and widen, increasing blood flow and lowering blood pressure.
Physiological Roles of Vasoconstriction
Vasoconstriction is essential for several normal body functions:
Regulating Blood Pressure: By narrowing blood vessels, vasoconstriction increases resistance to blood flow, which helps stabilize or raise blood pressure when needed.
Controlling Blood Distribution: It directs blood flow to organs and tissues that require more oxygen and nutrients by constricting vessels in less critical areas.
Maintaining Body Temperature: In cold environments, vasoconstriction reduces blood flow to the skin surface, minimizing heat loss and helping to preserve core body temperature.
Reducing Blood Loss: After injury, vasoconstriction helps limit bleeding by narrowing vessels near the wound site, though this effect is temporary to allow healing processes to proceed.
Mechanisms Behind Vasoconstriction
Vasoconstriction is controlled by several factors:
Nervous System: The sympathetic nervous system activates vasomotor nerves that release norepinephrine, which binds to alpha-adrenergic receptors on smooth muscle cells, causing contraction.
Hormones: Substances like endothelin and angiotensin II are potent vasoconstrictors released into the bloodstream to regulate vascular tone.
Local Factors: The blood vessels themselves can respond to changes in pressure or chemical signals, adjusting their diameter accordingly (myogenic response).
Causes And Triggers of Vasoconstriction
Vasoconstriction can be triggered by a variety of internal and external factors:
Cold Exposure: The body constricts vessels near the skin to reduce heat loss.
Stress: Activation of the sympathetic nervous system during stress leads to vasoconstriction.
Certain Foods and Substances: Excessive intake of caffeine, salt, and stimulants can induce vasoconstriction.
Medications: Some drugs, including nasal decongestants and antihistamines, cause vasoconstriction as part of their therapeutic effect.
Pathological Conditions: Disorders like hypertension, Raynaud’s disease, and reversible cerebral vasoconstriction syndrome involve abnormal or excessive vasoconstriction.
Effects of Vasoconstriction on the Body
When blood vessels constrict, the following physiological changes occur:
Increased Blood Pressure: Narrower vessels increase resistance, making the heart work harder to pump blood.
Reduced Blood Flow: Tissues downstream receive less blood, which can be protective or harmful depending on the context.
Potential Tissue Ischemia: Prolonged or excessive vasoconstriction may limit oxygen delivery, leading to tissue damage, as seen in conditions like Raynaud’s phenomenon.
Clinical Significance And Health Implications
While vasoconstriction is crucial for normal bodily functions, abnormal or prolonged vasoconstriction can contribute to health problems:
Hypertension: Chronic vasoconstriction raises blood pressure, increasing the risk of cardiovascular diseases such as heart attack and stroke.
Headaches and Migraines: Vasoconstriction in cerebral vessels can trigger headache pain.
Peripheral Vascular Disorders: Excessive vasoconstriction can cause symptoms like cold extremities, numbness, and in severe cases, tissue damage.
Drug Side Effects: Some medications and substances that induce vasoconstriction may exacerbate cardiovascular risks, especially in people with pre-existing conditions.
Diagnosis And Measurement
Vasoconstriction can be evaluated by measuring blood flow and vessel diameter using techniques such as Doppler ultrasound. Studies have shown that vasoconstrictor responses vary between limbs, with legs often exhibiting stronger vasoconstriction than arms in response to pressure changes.
Management and Treatment
Treatment of vasoconstriction depends on its cause:
Lifestyle Adjustments: Avoiding triggers like cold exposure, stress, excessive caffeine, and salt intake can help manage vasoconstriction.
Medications: Vasodilators are prescribed to relax blood vessels and improve blood flow in cases of chronic vasoconstriction or hypertension.
Symptom Relief: For cold-induced vasoconstriction, warming techniques are effective. Stress-related vasoconstriction can be managed with relaxation methods such as deep breathing, yoga, or meditation.
Avoiding Certain Drugs: People with high blood pressure should avoid over-the-counter decongestants that cause vasoconstriction.
Preventive Measures
To maintain healthy blood vessels and prevent excessive vasoconstriction:
Maintain a balanced diet low in salt and stimulants.
Manage stress through regular relaxation techniques.
Dress appropriately for cold weather to prevent unnecessary vasoconstriction.
Monitor blood pressure regularly and follow medical advice if hypertensive.
Conclusion
Vasoconstriction is a fundamental physiological mechanism that helps regulate blood pressure, blood flow, and body temperature. It involves the narrowing of blood vessels through smooth muscle contraction, controlled by nervous and hormonal signals. While it is essential for maintaining homeostasis, excessive or prolonged vasoconstriction can lead to serious health issues such as hypertension and tissue ischemia. Understanding the causes, effects, and management of vasoconstriction is crucial for cardiovascular health and effective clinical care.
Related topics: