Bradycardia is a condition where the heart rate falls below 60 beats per minute. It can be physiological or pathological. In some individuals, especially athletes, bradycardia may not cause symptoms. However, in others, it can lead to fatigue, dizziness, syncope, hypotension, and even cardiac arrest.
Prompt recognition and treatment of symptomatic bradycardia are essential. Medications that increase heart rate or improve cardiac output are often used. Dopamine is one of the pharmacologic agents employed in such cases.
What Is Dopamine?
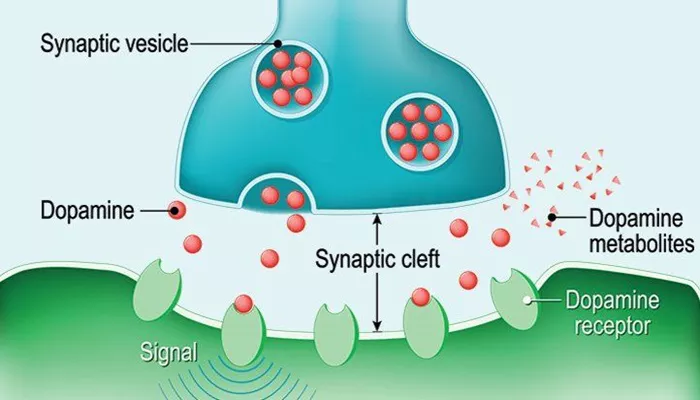
Dopamine is a catecholamine. It acts as both a neurotransmitter and a medication. It stimulates different adrenergic and dopaminergic receptors depending on the dose. It has both inotropic and chronotropic effects. These properties make it useful in treating cardiovascular emergencies.
Dopamine Receptor Activity by Dose
Low Dose (1–2 mcg/kg/min)
At low doses, dopamine primarily activates dopamine-1 receptors in the renal, mesenteric, coronary, and cerebral vascular beds. This causes vasodilation and improved perfusion, especially in the kidneys. It does not significantly affect heart rate or blood pressure.
Medium Dose (2–10 mcg/kg/min)
At this range, dopamine stimulates beta-1 adrenergic receptors. It increases myocardial contractility (positive inotropy) and heart rate (positive chronotropy). These effects are critical in treating bradycardia and hypotension associated with decreased cardiac output.
High Dose (>10 mcg/kg/min)
At high doses, dopamine activates alpha-1 receptors. This causes vasoconstriction, increasing systemic vascular resistance and blood pressure. This effect may help maintain perfusion in hypotensive states, although it also increases afterload.
Why Use Dopamine in Bradycardia?
Improves Heart Rate
Dopamine’s beta-1 effects at moderate doses directly increase the heart rate. This makes it suitable for patients with symptomatic bradycardia who are unresponsive to initial interventions like atropine.
Enhances Cardiac Output
In bradycardic patients with low cardiac output, dopamine enhances myocardial contractility. This raises stroke volume and overall perfusion, helping to stabilize vital signs.
Supports Blood Pressure
Bradycardia often coexists with hypotension. Dopamine increases both heart rate and systemic vascular resistance, helping to restore adequate blood pressure in emergencies.
Useful in Certain Emergency Situations
According to the American Heart Association (AHA), dopamine is recommended in cases of symptomatic bradycardia unresponsive to atropine and when transcutaneous pacing is not immediately available. It serves as a bridge therapy until definitive treatment, such as pacing, is initiated.
Clinical Indications for Dopamine in Bradycardia
Unstable Bradycardia
Dopamine is indicated in patients with bradycardia who show signs of hemodynamic compromise, such as hypotension, altered mental status, chest pain, or signs of shock.
Failure of First-Line Therapy
Atropine is the initial drug of choice. If bradycardia persists after adequate atropine dosing, dopamine becomes the next recommended pharmacologic option.
Unavailable or Ineffective Pacing
In settings where transcutaneous or transvenous pacing cannot be performed or fails, dopamine provides a pharmacologic solution to stabilize the patient.
Dosage Guidelines
The standard recommended dopamine dose for bradycardia is:
- Start at 2–10 mcg/kg/min IV infusion
- Titrate to the desired heart rate and blood pressure response
The infusion should be adjusted based on patient response. Continuous cardiac and hemodynamic monitoring is necessary.
Administration and Monitoring
Route of Administration
Dopamine is administered intravenously. A central line is preferred for prolonged use due to the risk of extravasation with peripheral lines.
Monitoring Parameters
Patients on dopamine require close monitoring:
- Heart rate and rhythm
- Blood pressure
- Urine output
- Signs of extravasation
Overstimulation can cause tachyarrhythmias and hypertension. The dose should be adjusted accordingly.
Potential Side Effects
Arrhythmias
High or even therapeutic doses of dopamine can cause tachyarrhythmias. These may include premature ventricular contractions (PVCs), atrial fibrillation, or ventricular tachycardia.
Hypertension
Dopamine can cause excessive vasoconstriction at higher doses. This may elevate blood pressure significantly, especially in volume-depleted patients.
Tissue Necrosis
Extravasation of dopamine can lead to local tissue damage and necrosis. Phentolamine may be used to treat extravasation injuries.
Contraindications and Cautions
Contraindications
- Pheochromocytoma
- Uncorrected tachyarrhythmias
- Known hypersensitivity to dopamine or its components
Use with Caution
- In patients with myocardial infarction: Dopamine increases myocardial oxygen demand
- In patients with volume depletion: Ensure fluid resuscitation before initiating dopamine
Comparison with Other Medications
Dopamine vs. Atropine
Atropine is the first-line drug for bradycardia. It works by inhibiting parasympathetic input to the heart. However, it may be ineffective in certain bradyarrhythmias, such as high-degree AV block. Dopamine is a second-line agent used when atropine fails.
Dopamine vs. Epinephrine
Both dopamine and epinephrine can be used in unstable bradycardia. Epinephrine acts more potently on alpha and beta receptors, which may lead to increased side effects. Dopamine is often preferred when a more titratable response is needed.
Dopamine vs. Pacing
Pacing remains the definitive treatment for many forms of bradycardia, especially complete heart block. Dopamine serves as a bridge therapy or temporary solution until pacing can be implemented.
Case Example
A 68-year-old man presents with dizziness, bradycardia (heart rate 38 bpm), and hypotension (BP 80/50 mmHg). Atropine 0.5 mg IV is administered with no effect. Transcutaneous pacing is not available. Dopamine is initiated at 5 mcg/kg/min.
Over the next 10 minutes, heart rate increases to 60 bpm and blood pressure stabilizes to 100/70 mmHg. The patient is then prepared for transvenous pacing.
Conclusion
Dopamine plays a key role in the management of symptomatic bradycardia, especially when first-line therapies are ineffective or unavailable. It enhances heart rate, cardiac output, and blood pressure. Dopamine is a valuable tool in the emergency management of bradycardia. Its use must be guided by careful monitoring and dose titration. Understanding its pharmacodynamics and clinical application ensures safe and effective treatment for patients in critical situations.
Related topics: