Unstable angina is a serious medical condition that requires prompt attention and management. It is a type of chest pain or discomfort that occurs when the heart muscle doesn’t receive enough oxygen-rich blood. Unlike stable angina, which typically occurs during physical activity or stress and improves with rest or medication, unstable angina can happen even at rest and is considered a medical emergency. In this article, we will explore the nature of unstable angina, its causes, symptoms, diagnosis, treatment options, and whether it can be cured.
Understanding Unstable Angina
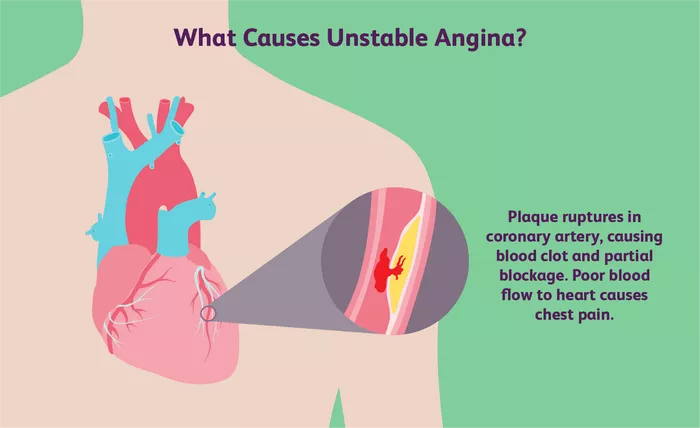
Unstable angina is often a sign of an impending heart attack (myocardial infarction). It occurs due to a partial blockage of the coronary arteries, which supply blood to the heart muscle. The reduced blood flow to the heart can lead to chest pain or discomfort, known as angina. Unstable angina is characterized by its unpredictability and may occur with increasing frequency, severity, and duration over time.
Causes of Unstable Angina
The primary cause of unstable angina is atherosclerosis, a condition where plaque builds up inside the coronary arteries, narrowing them and reducing blood flow. Plaque is made up of cholesterol, fatty substances, calcium, and other substances found in the blood. When plaque ruptures or becomes unstable, it can trigger the formation of blood clots that further block the arteries, leading to unstable angina or a heart attack.
Other risk factors for unstable angina include:
1. Smoking: Tobacco use damages the blood vessels and increases the risk of atherosclerosis.
2. High Blood Pressure: Hypertension puts strain on the heart and arteries, contributing to plaque formation.
3. High Cholesterol: Elevated levels of LDL cholesterol (“bad” cholesterol) can lead to plaque buildup in the arteries.
4. Diabetes: Uncontrolled diabetes can damage blood vessels and increase the risk of atherosclerosis.
5. Obesity: Excess body weight puts additional strain on the heart and increases the risk of heart disease.
6. Physical Inactivity: Lack of exercise contributes to obesity, high blood pressure, and other risk factors for heart disease.
7. Family History: A family history of heart disease increases the likelihood of developing unstable angina.
8. Stress: Chronic stress can contribute to high blood pressure and unhealthy coping behaviors like overeating or smoking.
Symptoms of Unstable Angina
The symptoms of unstable angina are similar to those of stable angina but are more severe and occur with less predictability. Common symptoms include:
- Chest pain or discomfort, often described as pressure, squeezing, heaviness, or tightness
- Pain that may radiate to the neck, jaw, shoulders, back, or arms
- Shortness of breath
- Nausea
- Sweating
- Dizziness or lightheadedness
It’s essential to seek immediate medical attention if you experience symptoms of unstable angina, as it can indicate a serious heart condition that requires urgent treatment.
Diagnosis of Unstable Angina
To diagnose unstable angina, your healthcare provider will conduct a thorough medical history, physical examination, and may order the following tests:
1. Electrocardiogram (ECG or EKG): This test records the electrical activity of your heart and can detect abnormalities indicative of unstable angina or a heart attack.
2. Blood Tests: Blood tests can measure cardiac enzymes, such as troponin, which are released into the bloodstream when the heart muscle is damaged.
3. Echocardiogram: This imaging test uses sound waves to create a picture of your heart’s structure and function, helping to assess blood flow and detect any abnormalities.
4. Stress Test: A stress test evaluates how your heart performs during physical activity, such as walking on a treadmill or using medication to simulate exercise when physical activity is not possible.
5. Coronary Angiography: This invasive procedure involves injecting contrast dye into the coronary arteries to visualize any blockages or narrowing.
Based on the results of these tests, your healthcare provider can determine if you have unstable angina and develop an appropriate treatment plan.
Treatment Options for Unstable Angina
The goal of treatment for unstable angina is to relieve symptoms, prevent complications, and reduce the risk of a heart attack. Treatment strategies may include:
Medications:
1. Nitroglycerin: Helps dilate blood vessels and improve blood flow to the heart.
2. Aspirin and Antiplatelet Medications: Reduce the risk of blood clots forming in the arteries.
3. Beta-Blockers: Lower heart rate and blood pressure, reducing the heart’s workload.
4. Statins: Lower cholesterol levels and reduce plaque buildup in the arteries.
5. Angiotensin-Converting Enzyme (ACE) Inhibitors or Angiotensin II Receptor Blockers (ARBs): Help relax blood vessels and lower blood pressure.
Lifestyle Changes:
1. Quitting Smoking: Smoking cessation is crucial for improving heart health and reducing the risk of complications.
2. Healthy Diet: A diet low in saturated fat, cholesterol, and sodium can help manage risk factors like high cholesterol and high blood pressure.
3. Regular Exercise: Physical activity strengthens the heart muscle, improves circulation, and helps maintain a healthy weight.
4. Stress Management: Techniques such as meditation, yoga, and deep breathing exercises can help reduce stress and improve overall well-being.
Medical Procedures:
1. Percutaneous Coronary Intervention (PCI): Also known as angioplasty, this procedure involves inserting a catheter with a balloon to open narrowed or blocked arteries and may include placing a stent to keep the artery open.
2. Coronary Artery Bypass Grafting (CABG): In severe cases where multiple arteries are blocked, CABG surgery may be necessary to create new routes for blood flow to the heart.
Can Unstable Angina Be Cured?
While unstable angina can be effectively managed and treated to reduce symptoms and prevent complications, it is not typically considered curable in the traditional sense. The underlying cause of unstable angina, such as atherosclerosis and coronary artery disease, may persist despite treatment. However, with proper medical care, lifestyle changes, and adherence to treatment plans, individuals with unstable angina can lead fulfilling lives and reduce their risk of experiencing serious cardiac events.
It’s important for individuals with unstable angina to work closely with their healthcare providers to develop a comprehensive treatment plan tailored to their needs. This may include regular follow-up appointments, monitoring of cardiac function and risk factors, and adjustments to medications or lifestyle recommendations as needed.
In conclusion, while unstable angina may not be cured outright, it can be effectively managed and controlled with appropriate medical intervention, lifestyle modifications, and ongoing care. Early diagnosis, prompt treatment, and proactive management of risk factors are essential for optimizing outcomes and reducing the risk of complications associated with this serious cardiac condition.