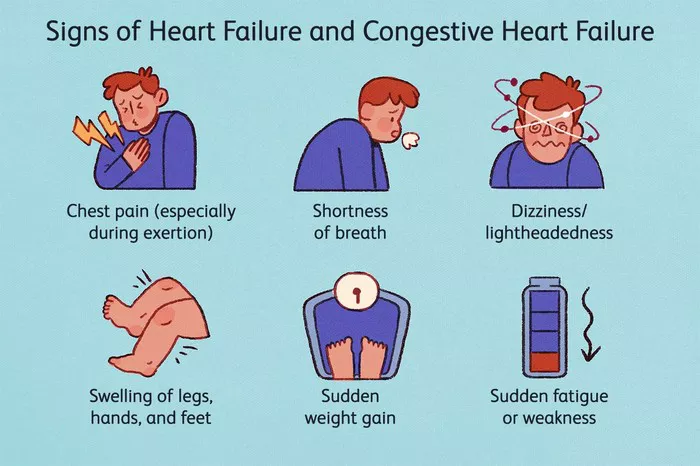
Congestive heart failure (CHF) is a chronic condition where the heart is unable to pump blood effectively, leading to a buildup of fluid in the body. This fluid retention can affect various organs, particularly the lungs, liver, and legs, causing symptoms such as shortness of breath, swelling, and fatigue. Managing fluid buildup is a key aspect of treating CHF, as excessive fluid can worsen heart failure and lead to complications like pulmonary edema or kidney damage. In this article, we will explore the different methods to remove excess fluid from the body in the context of congestive heart failure.
Understanding Congestive Heart Failure (CHF)
CHF occurs when the heart’s ability to pump blood is impaired, often due to conditions like coronary artery disease, high blood pressure, or previous heart attacks. As a result, blood backs up in the veins, causing fluid to accumulate in different parts of the body. This fluid buildup leads to symptoms like swelling in the legs, abdomen, and around the lungs, making it difficult for individuals with CHF to breathe or perform daily activities.
Fluid retention can happen when the kidneys do not receive enough blood flow to filter out excess fluid. As a result, the body starts retaining more sodium and water, leading to even more fluid buildup.
Key Goals in Treating Fluid Retention in CHF
The primary goal of treatment is to reduce fluid buildup while improving the heart’s ability to pump blood. This involves a combination of medications, lifestyle changes, and, in some cases, medical procedures. Let’s explore these treatment options in detail.
1. Diuretics (Fluid Removal Medications)
One of the most common and effective ways to get rid of fluid in CHF is by using diuretics, also known as water pills. These medications help the kidneys remove excess fluid and sodium from the body through urine. By reducing the volume of fluid in the body, diuretics help alleviate symptoms of fluid retention, such as swelling and shortness of breath.
There are different types of diuretics, including:
Loop Diuretics
Loop diuretics, such as furosemide (Lasix), are the most commonly prescribed for CHF. They work by blocking the reabsorption of sodium and chloride in the kidneys’ loop of Henle, allowing more fluid to be excreted. These diuretics are potent and effective at reducing fluid buildup in patients with severe heart failure.
Thiazide Diuretics
Thiazide diuretics, such as hydrochlorothiazide, are often used in combination with loop diuretics to manage mild fluid retention. They work by inhibiting sodium reabsorption in the kidneys’ distal tubule, but they are generally less effective than loop diuretics.
Potassium-Sparing Diuretics
Potassium-sparing diuretics, such as spironolactone, help the body remove excess fluid without losing potassium, which can be a concern with other diuretics. Spironolactone also has beneficial effects in heart failure by blocking aldosterone, a hormone that can worsen fluid retention.
How Diuretics Help:
- Reduce swelling and fluid buildup
- Improve breathing and lung function
- Enhance the heart’s ability to pump blood by reducing the volume of fluid the heart has to manage
2. Sodium and Fluid Restrictions
In addition to medications, patients with CHF are often advised to limit their sodium intake and fluid consumption. High sodium levels can cause the body to retain more fluid, worsening symptoms of fluid retention.
Sodium Restriction
Limiting sodium intake is crucial for controlling fluid buildup. The American Heart Association recommends that individuals with CHF consume no more than 2,000 mg of sodium per day. This can be achieved by avoiding processed foods, canned goods, salty snacks, and restaurant meals, which are often high in sodium.
Fluid Restriction
In some cases, patients may be instructed to limit their fluid intake, especially during periods of worsening heart failure.
This helps to prevent the kidneys from becoming overloaded with fluid. A typical fluid restriction may range from 1.5 to 2 liters per day, but it varies based on the severity of the heart failure and the patient’s specific condition.
3. ACE Inhibitors and ARBs (Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers)
ACE inhibitors and ARBs are classes of medications commonly used to treat heart failure. While their primary function is to relax blood vessels and reduce the workload on the heart, they can also help reduce fluid buildup indirectly.
ACE Inhibitors (e.g., Enalapril, Lisinopril)
ACE inhibitors block the conversion of angiotensin I to angiotensin II, a hormone that causes blood vessels to constrict. By reducing blood vessel constriction, ACE inhibitors help lower blood pressure and reduce the strain on the heart. This leads to better blood flow to the kidneys, allowing them to eliminate excess fluid more effectively.
ARBs (e.g., Losartan, Valsartan)
ARBs work similarly to ACE
inhibitors by blocking the effects of angiotensin II, but they do so in a slightly different way. They are often prescribed to patients who cannot tolerate ACE inhibitors due to side effects such as a persistent cough.
How ACE Inhibitors and ARBs Help:
- Lower blood pressure and reduce fluid retention
- Improve kidney function by improving blood flow
- Reduce strain on the heart and prevent fluid buildup
4. Beta-Blockers
Beta-blockers, such as carvedilol and metoprolol, are another important class of medications used in the treatment of CHF.
These medications block the effects of adrenaline, a hormone that can increase heart rate and blood pressure. By reducing the heart’s workload, beta-blockers can prevent fluid buildup and improve overall heart function.
How Beta-Blockers Help:
- Decrease heart rate and blood pressure
- Improve the heart’s pumping ability
- Prevent the worsening of fluid retention
5. Aldosterone Antagonists
Aldosterone antagonists, such as spironolactone, are a type of potassium-sparing diuretic. They work by blocking aldosterone, a hormone that can lead to fluid retention. Aldosterone antagonists are often used in patients with advanced heart failure to improve symptoms and reduce the risk of hospitalization.
How Aldosterone Antagonists Help:
- Block aldosterone to prevent fluid retention
- Improve symptoms of heart failure
- Reduce the risk of heart failure complications
6. Mechanical Devices and Procedures
In some cases, medical procedures or mechanical devices may be necessary to manage fluid retention in patients with severe CHF.
Implantable Cardioverter-Defibrillators (ICDs)
While ICDs are primarily used to prevent life-threatening arrhythmias, they can also help improve heart function and reduce fluid buildup by providing electrical shocks to restore normal rhythm in patients with heart failure.
Left Ventricular Assist Devices (LVADs)
An LVAD is a mechanical pump that is used to help the heart pump blood more effectively in patients with advanced heart failure. By improving heart function, LVADs can reduce fluid retention and improve overall symptoms.
Ultrafiltration
Ultrafiltration is a procedure used to remove excess fluid from the body by passing blood through a filter, similar to dialysis.
This treatment is typically used in patients with acute heart failure who do not respond well to diuretics.
How Mechanical Devices and Procedures Help:
- Improve heart function and reduce fluid buildup
- Provide temporary support until a heart transplant is possible
- Offer alternative solutions when medications are insufficient
Conclusion
Managing fluid retention is a crucial aspect of treating congestive heart failure. A combination of medications, lifestyle changes, and sometimes medical procedures can help remove excess fluid and improve the patient’s quality of life.
Diuretics, sodium and fluid restrictions, ACE inhibitors, ARBs, beta-blockers, and aldosterone antagonists are commonly used to manage fluid retention and support heart function. For patients with severe CHF, mechanical devices and procedures like LVADs and ultrafiltration may be necessary to control symptoms and improve heart function.
Related topics: