A splenorenal shunt (SRS) is a type of abnormal vascular connection between the splenic vein and the left renal vein. This rare condition allows blood from the spleen to bypass the liver and flow directly into the kidneys. Such a connection can occur due to a variety of causes, often related to portal hypertension or liver disease. Understanding the causes of a splenorenal shunt is critical for diagnosing and treating associated complications such as variceal bleeding, kidney dysfunction, and hypertension. This article will delve into the key causes of splenorenal shunt, the pathophysiology behind it, and its potential clinical implications.
Understanding Splenorenal Shunt
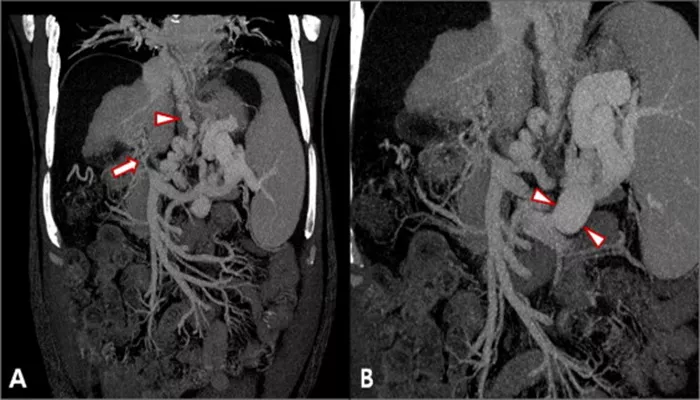
A splenorenal shunt forms when there is an abnormal communication between the splenic vein and the renal vein. The splenic vein typically carries blood from the spleen and joins the superior mesenteric vein to form the portal vein, which then directs blood into the liver. In a splenorenal shunt, the blood bypasses the liver and enters the left renal vein, and from there, it flows into the systemic circulation. This bypass occurs due to the formation of collateral vessels in response to increased resistance to blood flow in the portal vein.
A splenorenal shunt is often associated with portal hypertension, a condition where increased pressure within the portal venous system leads to the formation of these collateral pathways. These shunts can be congenital or acquired, with the latter being more common in adults, particularly those with cirrhosis or liver fibrosis.
Key Causes of Splenorenal Shunt
1. Portal Hypertension
Portal hypertension is the most common cause of a splenorenal shunt.
It occurs when there is increased pressure in the portal vein, which usually results from liver cirrhosis, hepatic fibrosis, or other liver diseases. In portal hypertension, the normal flow of blood through the liver becomes obstructed, forcing blood to find alternative routes. As a result, collateral vessels, such as the splenorenal shunt, form to reroute blood away from the liver and towards the systemic circulation.
Cirrhosis: Cirrhosis is the most frequent cause of portal hypertension.
In cirrhosis, the liver tissue becomes scarred and fibrotic, disrupting normal blood flow through the liver. As a compensatory mechanism, collateral blood vessels, including splenorenal shunts, develop.
Hepatic Fibrosis: Fibrosis of the liver tissue, often from chronic alcohol abuse, hepatitis, or fatty liver disease, can also increase portal pressure, leading to the formation of a splenorenal shunt.
Schistosomiasis: This parasitic infection, particularly prevalent in tropical and subtropical regions, can cause fibrosis in the liver and portal hypertension, resulting in splenorenal shunting.
2. Chronic Liver Disease
Chronic liver diseases are major contributors to the development of splenorenal shunts due to their association with portal hypertension.
Conditions such as hepatitis, fatty liver disease, and primary biliary cirrhosis can lead to liver dysfunction and vascular changes within the portal venous system.
Non-Alcoholic Fatty Liver Disease (NAFLD): This increasingly common condition, related to metabolic syndrome and obesity, can progress to cirrhosis, and portal hypertension. As liver function declines, splenorenal shunts may form.
Chronic Hepatitis B and C: These viral infections can cause long-term liver inflammation, eventually leading to cirrhosis and the development of portal hypertension. The associated pressure in the portal system can result in the formation of shunts.
3. Trauma or Injury to the Spleen or Renal Vein
In rare cases, trauma or injury to the spleen or renal vein may lead to the development of a splenorenal shunt. A direct injury or surgery in the abdominal area could cause disruption in normal venous circulation, leading to the formation of abnormal shunts.
Blunt Abdominal Trauma: Blunt trauma, such as a car accident, can damage the spleen or renal vein. If these vessels are injured, a collateral vessel may form to compensate for the lost or damaged venous pathways, leading to a splenorenal shunt.
Post-surgical Complications: In certain cases, abdominal surgeries, including those involving the spleen or kidneys, can inadvertently cause the formation of abnormal vascular connections, including a splenorenal shunt.
4. Congenital Abnormalities
Although less common, some individuals may be born with a splenorenal shunt due to congenital vascular malformations. In such cases, an abnormal connection between the splenic vein and the renal vein is present from birth, although it may remain asymptomatic until later in life. These congenital shunts are typically identified during investigations for other conditions, such as unexplained portal hypertension or kidney problems.
Congenital Portal Vein Malformations: Some individuals may have abnormal development of the portal vein system during fetal development, leading to the formation of a splenorenal shunt. These malformations can cause an increase in portal pressure and alter normal blood flow patterns.
Arteriovenous Malformations: Rarely, the presence of arteriovenous malformations (AVMs) in the splenic or renal vessels can predispose individuals to the development of shunts, including splenorenal shunts.
5. Tumors and Malignancies
Certain tumors, particularly those of the liver or spleen, can contribute to the formation of a splenorenal shunt. Malignant growths can obstruct normal venous pathways or cause increased pressure within the portal system, leading to the development of collateral vessels.
Hepatocellular Carcinoma (HCC): A primary liver cancer, HCC, can cause cirrhosis and subsequent portal hypertension, increasing the risk of splenorenal shunts.
Splenic Malignancies: Tumors in the spleen can obstruct the normal venous flow and create an environment conducive to shunt formation.
Pancreatic Cancer: Malignant tumors of the pancreas may invade surrounding vascular structures, including the splenic vein, contributing to the development of a splenorenal shunt.
6. Idiopathic Causes
In some instances, a splenorenal shunt may occur without an identifiable underlying cause. These cases are classified as idiopathic, where no clear reason for the formation of the shunt can be determined. However, even in such cases, portal hypertension is often implicated as a contributing factor.
Idiopathic Portal Hypertension: Some individuals may develop portal hypertension and a splenorenal shunt without any apparent liver disease or other identifiable causes. This condition, while rare, underscores the complexity of vascular malformations in the body.
Clinical Implications of Splenorenal Shunt
1. Risk of Variceal Bleeding
The formation of a splenorenal shunt may be associated with the development of esophageal varices or other varices in the gastrointestinal tract. These varices are dilated blood vessels that can rupture and cause severe bleeding. Blood bypassing the liver, where it is typically detoxified, may lead to the accumulation of toxins and contribute to liver failure.
2. Renal Dysfunction
In some cases, the abnormal blood flow caused by a splenorenal shunt can lead to renal complications. Blood entering the kidneys without passing through the liver can alter normal kidney function, leading to conditions such as renal insufficiency or hypertension.
3. Portal Hypertension Complications
As portal hypertension is the main driver of splenorenal shunt formation, its complications are significant. These may include ascites, encephalopathy, and other signs of liver failure.
Conclusion
A splenorenal shunt is a rare but clinically significant vascular anomaly often caused by portal hypertension or chronic liver disease. Its formation can be triggered by various factors, including cirrhosis, hepatic fibrosis, traumatic injury, congenital abnormalities, and malignancies. Understanding the underlying causes and the pathophysiology of splenorenal shunt is crucial for diagnosing the condition, managing its complications, and improving patient outcomes. Early detection and intervention are key to preventing severe complications such as variceal bleeding or renal dysfunction.
Related topics: