Splenic varices are enlarged veins in the spleen caused by increased pressure within the portal vein system. This condition is often associated with liver diseases or other factors that disrupt normal blood flow in the abdomen. Although splenic varices are less commonly discussed than other types of varices, they are an important medical issue and can have serious health consequences if not properly managed. In this article, we will explore the causes, risk factors, and mechanisms behind splenic varices, with a particular focus on understanding how these factors contribute to the development of this condition.
What Are Splenic Varices?
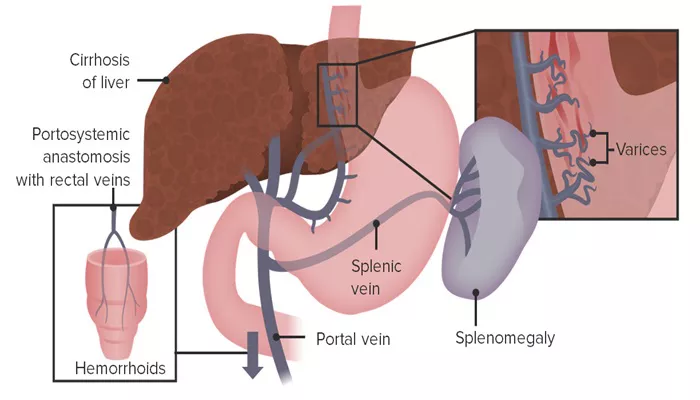
Splenic varices are abnormal veins that form in and around the spleen. These varices develop as a result of increased pressure in the portal vein, a major blood vessel that carries blood from the intestines and spleen to the liver. When the liver becomes damaged or obstructed, the blood flow is impeded, causing blood to back up into surrounding veins, including those in the spleen. Over time, this increased pressure causes the veins in the spleen to enlarge and become varices.
Unlike esophageal varices, which are commonly associated with liver cirrhosis, splenic varices are a relatively rare condition. However, they can still lead to significant complications if not recognized and treated.
The Main Causes of Splenic Varices
1. Portal Hypertension
Portal hypertension is the most common cause of splenic varices. This condition occurs when there is increased pressure within the portal venous system. The portal vein is responsible for carrying blood from the intestines, spleen, and pancreas to the liver. When blood flow through the liver is obstructed, such as in the case of cirrhosis or fibrosis, pressure begins to build up in the portal vein.
As a result of this elevated pressure, the body seeks alternative pathways for blood to flow back to the heart. These collateral veins develop around the liver, spleen, and stomach. In some cases, these veins in the spleen become significantly enlarged, leading to splenic varices.
2. Liver Cirrhosis
Liver cirrhosis is a leading cause of portal hypertension. In cirrhosis, the liver tissue becomes scarred due to chronic liver damage, which can be caused by conditions such as hepatitis, alcohol abuse, or non-alcoholic fatty liver disease (NAFLD).
The scar tissue obstructs the normal flow of blood through the liver, leading to increased pressure in the portal vein. This results in the development of varices, including splenic varices, as the body compensates for the blocked blood flow.
Cirrhosis not only impairs liver function but also disrupts the vascular structures within the liver, making it one of the most significant causes of splenic varices.
3. Splenic Vein Thrombosis
Splenic vein thrombosis (SVT) refers to the formation of a blood clot in the splenic vein. This can be caused by a variety of factors, such as inflammation, infection, or trauma. When a clot forms in the splenic vein, it obstructs blood flow, leading to a backup of blood in the spleen and the development of splenic varices.
SVT can occur as a complication of liver diseases, such as cirrhosis, or as a result of abdominal conditions like pancreatitis.
Other conditions, including cancer and certain blood clotting disorders, can also increase the risk of splenic vein thrombosis.
4. Pancreatitis and Pancreatic Cancer
Pancreatitis, which refers to inflammation of the pancreas, can be another cause of splenic varices. The pancreas is located near the spleen, and inflammation or damage to this organ can affect the blood vessels that surround it. If the inflammation causes narrowing or obstruction of the splenic vein, it can lead to splenic vein thrombosis and portal hypertension, which in turn may result in the formation of splenic varices.
Pancreatic cancer can also contribute to splenic varices. As the tumor grows, it can obstruct the surrounding blood vessels, including the splenic vein, leading to portal hypertension and the development of varices.
5. Schistosomiasis
Schistosomiasis is a parasitic infection that affects millions of people worldwide, particularly in tropical and subtropical regions. The parasites, called schistosomes, migrate to the liver and intestines, causing inflammation and damage to the blood vessels. Over time, this damage can lead to scarring and obstruction of the portal vein, resulting in portal hypertension.
In regions where schistosomiasis is endemic, it is one of the leading causes of splenic varices. The chronic inflammation caused by schistosomiasis can lead to significant liver damage, making portal hypertension and varices more likely.
6. Congenital Vascular Abnormalities
Some individuals are born with abnormalities in the vascular structures of the abdomen, including the veins of the spleen.
These congenital conditions can predispose individuals to the development of splenic varices. Although less common, congenital vascular malformations can lead to abnormal blood flow in the portal vein and spleen, causing increased pressure and the formation of varices.
7. Extrahepatic Portal Vein Obstruction
Extrahepatic portal vein obstruction (EHPVO) is a condition in which the portal vein becomes blocked outside the liver, usually due to clot formation or fibrosis. This blockage leads to portal hypertension and can result in the formation of splenic varices.
EHPVO can be caused by a variety of factors, including thrombosis of the portal vein, trauma, or chronic conditions that affect blood clotting. When the portal vein is obstructed, blood is rerouted through collateral veins, including those in the spleen, leading to splenic varices.
Risk Factors for Splenic Varices
Several factors can increase the risk of developing splenic varices.
These include:
Chronic liver diseases: Conditions such as cirrhosis, hepatitis, and fatty liver disease are major risk factors for portal hypertension and splenic varices.
Pancreatic disorders: Pancreatitis and pancreatic cancer can obstruct blood flow and contribute to the development of splenic varices.
Blood clotting disorders: Conditions that increase the risk of blood clot formation, such as thrombophilia, can lead to splenic vein thrombosis and subsequent varices.
Age: Older individuals are more likely to develop liver diseases and other conditions that contribute to splenic varices.
Infections: Infections like schistosomiasis can increase the risk of portal hypertension and splenic varices, particularly in endemic areas.
Genetic factors: Some congenital vascular malformations may predispose individuals to splenic varices.
Symptoms and Complications of Splenic Varices
Most individuals with splenic varices do not experience symptoms unless the varices become significantly enlarged or rupture. When symptoms do occur, they may include:
Abdominal pain: This pain can be caused by the enlargement of the spleen (splenomegaly) or the rupture of varices.
Enlarged spleen: A palpable swelling or mass in the left upper abdomen can be a sign of splenic varices.
Signs of internal bleeding: If the varices rupture, they can cause severe internal bleeding, leading to shock, dizziness, and a rapid drop in blood pressure.
If left untreated, splenic varices can lead to serious complications, including hemorrhage, splenic rupture, and long-term liver damage.
Diagnosis and Treatment
Diagnosing splenic varices typically involves imaging studies, such as ultrasound, CT scans, or MRI, to assess the size of the spleen and the blood vessels. A Doppler ultrasound can be used to assess blood flow in the portal vein and detect any signs of portal hypertension.
Treatment of splenic varices depends on the underlying cause and the severity of the condition. Management strategies may include:
Medications: Beta-blockers and other medications to reduce portal pressure may be prescribed.
Endoscopic procedures: If bleeding occurs, endoscopic procedures such as banding or sclerotherapy may be used to control the varices.
Surgical intervention: In some cases, surgical procedures may be required to treat portal hypertension or to manage complications like ruptured varices.
Liver transplantation: If liver disease is the underlying cause, a liver transplant may be considered in severe cases.
Conclution
Splenic varices are a serious condition caused by increased pressure in the portal venous system. They are often a result of liver diseases such as cirrhosis, splenic vein thrombosis, or other factors that disrupt normal blood flow. Early diagnosis and treatment are essential to managing this condition and preventing complications like bleeding or spleen rupture.
Related topics: