Myocardial inflammation, commonly referred to as myocarditis, is a critical condition characterized by inflammation of the heart muscle (myocardium). It can lead to severe complications, including heart failure, arrhythmias, and sudden cardiac death. Accurate diagnosis and coding of myocarditis are essential for effective treatment, epidemiological tracking, and healthcare reimbursement. The International Classification of Diseases, 10th Revision (ICD-10), provides a standardized coding system for various medical conditions, including myocarditis. This article will explore the ICD-10 codes associated with myocardial inflammation, the importance of accurate coding, and the clinical implications of myocarditis.
Understanding Myocarditis
Definition of Myocarditis
Myocarditis is defined as inflammation of the myocardium, which can occur due to various etiological factors, including infectious agents, autoimmune conditions, toxic exposures, and more. The inflammation can damage the heart muscle, impairing its ability to pump blood effectively and leading to a range of clinical manifestations.
Epidemiology
Myocarditis is not a rare condition; it affects approximately 10 to 20 individuals per 100,000 annually. The incidence can vary based on geographical location, age, and underlying health conditions. It is most commonly observed in young adults and adolescents, particularly following viral infections. The recent COVID-19 pandemic has highlighted the increasing recognition of myocarditis as a complication of viral infections, emphasizing the need for awareness and prompt intervention.
Clinical Presentation
The clinical presentation of myocarditis can vary widely among patients. Common symptoms include:
Chest Pain: Often described as sharp or pressure-like, chest pain can mimic the symptoms of myocardial ischemia.
Shortness of Breath: Patients may experience dyspnea on exertion or at rest, indicating impaired cardiac function.
Fatigue: Unusual fatigue is common and may not improve with rest.
Palpitations: Irregular heartbeats or a racing heart can occur due to arrhythmias.
Swelling: Peripheral edema may develop due to fluid retention and heart failure.
Diagnosis
Diagnosing myocarditis involves a combination of clinical evaluation, imaging studies, and laboratory tests. Key components of the diagnostic process include:
History and Physical Examination: A thorough history and physical examination are essential to assess symptoms and identify risk factors.
Electrocardiogram (ECG): An ECG can reveal arrhythmias and other abnormalities indicative of myocarditis.
Cardiac Biomarkers: Elevated levels of troponin and B-type natriuretic peptide (BNP) can indicate myocardial injury and heart failure.
Echocardiography: This imaging modality helps assess cardiac structure and function, identifying wall motion abnormalities and ventricular function.
Cardiac Magnetic Resonance Imaging (MRI): Cardiac MRI is considered the gold standard for diagnosing myocarditis, providing detailed images of myocardial inflammation and edema.
Endomyocardial Biopsy: In select cases, a biopsy may be performed to obtain tissue for histological examination.
ICD-10 Coding for Myocardial Inflammation
Overview of ICD-10
The International Classification of Diseases, 10th Revision (ICD-10), is a coding system developed by the World Health Organization (WHO) to standardize the classification of diseases and health conditions. The ICD-10 provides codes for various medical conditions, which are used for clinical documentation, billing, and statistical purposes. Accurate coding is essential for effective healthcare management, research, and epidemiological tracking.
ICD-10 Codes for Myocarditis
In the ICD-10 coding system, myocarditis is classified under the category of inflammatory diseases of the heart. The relevant codes for myocarditis include:
I40.0: Myocarditis due to infectious disease
I40.1: Myocarditis due to non-infectious disease
I40.8: Other myocarditis
I40.9: Myocarditis, unspecified
I40.0 – Myocarditis Due to Infectious Disease
This code is used when myocarditis is caused by an infectious agent, such as a virus or bacteria. Common infectious causes include:
Viral Myocarditis: Often caused by viruses like Coxsackievirus, adenovirus, parvovirus B19, and influenza virus.
Bacterial Myocarditis: Can occur due to bacteria such as Streptococcus, Staphylococcus, and Borrelia burgdorferi.
Fungal Myocarditis: Rare but can occur in immunocompromised patients due to fungi like Candida and Aspergillus.
I40.1 – Myocarditis Due to Non-Infectious Disease
This code is used when myocarditis is attributed to non-infectious causes, such as autoimmune diseases, toxic exposures, or drug reactions. Common non-infectious causes include:
Autoimmune Conditions: Conditions like systemic lupus erythematosus (SLE) and rheumatoid arthritis can lead to myocarditis.
Toxic Exposures: Chronic alcohol consumption and certain medications can induce myocarditis.
Giant Cell Myocarditis: A rare form of myocarditis characterized by the presence of multinucleated giant cells.
I40.8 – Other Myocarditis
This code is used for other specified forms of myocarditis that do not fit the criteria for the above categories. It can include atypical presentations or rare forms of myocarditis.
I40.9 – Myocarditis, Unspecified
This code is used when the specific cause of myocarditis is unknown or not specified. It is important to use this code when the clinical details are insufficient to determine the exact etiology.
Importance of Accurate ICD-10 Coding
Accurate ICD-10 coding for myocardial inflammation is crucial for several reasons:
Clinical Documentation: Proper coding ensures that the patient’s medical record accurately reflects their condition, which is essential for ongoing care and treatment planning.
Reimbursement: Accurate coding is necessary for healthcare providers to receive appropriate reimbursement from insurance companies and government programs. Incorrect coding can lead to claim denials or underpayment.
Epidemiological Tracking: ICD-10 codes are used for public health surveillance and research. Accurate coding helps track the incidence and prevalence of myocarditis, informing healthcare policy and resource allocation.
Quality of Care: Accurate coding allows for better data collection and analysis, which can lead to improved quality of care and outcomes for patients with myocarditis.
Clinical Implications of Myocarditis
Complications
Myocarditis can lead to several serious complications, including:
Heart Failure: The inflammation can impair the heart’s ability to pump blood, leading to heart failure. This can manifest as dyspnea, fatigue, and fluid retention.
Arrhythmias: Myocarditis can disrupt the heart’s electrical conduction system, leading to arrhythmias. Patients may experience palpitations, dizziness, or syncope.
Sudden Cardiac Death: In severe cases, myocarditis can lead to sudden cardiac death, particularly in young individuals without prior heart disease.
Dilated Cardiomyopathy: Prolonged inflammation can lead to structural changes in the heart, resulting in dilated cardiomyopathy and chronic heart failure.
Treatment Options
The management of myocarditis depends on the underlying cause and severity of the condition. Key treatment options include:
Symptomatic Treatment: This may include diuretics to manage fluid overload, ACE inhibitors to improve cardiac output, and beta-blockers to control heart rate.
Immunosuppressive Therapy: In cases of autoimmune myocarditis, corticosteroids or other immunosuppressants may be initiated to reduce inflammation.
Antiviral Therapy: If a viral cause is suspected, antiviral therapy may be considered, although its efficacy is variable.
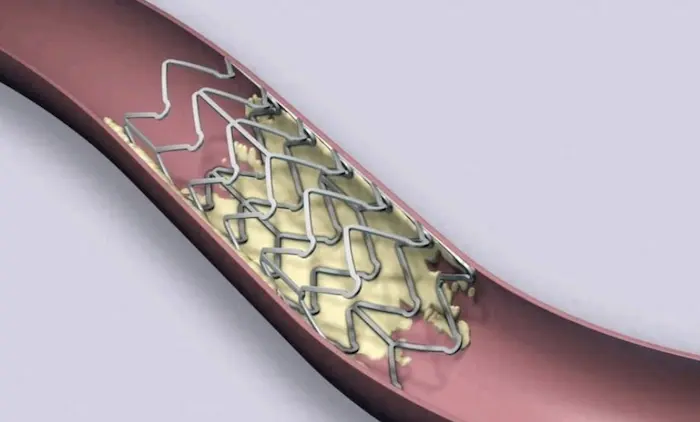
Advanced Interventions: In cases of severe heart failure or life-threatening arrhythmias, advanced interventions such as mechanical circulatory support or cardiac transplantation may be necessary.
Prognosis
The prognosis of myocarditis varies widely depending on the underlying cause, severity of inflammation, and timeliness of treatment. Many patients recover fully with appropriate management, while others may experience long-term complications such as heart failure or arrhythmias. Early recognition and intervention are crucial for improving outcomes in patients with myocarditis.
Conclusion
Myocardial inflammation, or myocarditis, is a complex condition with a diverse range of etiological factors. Understanding the ICD-10 codes associated with myocarditis is essential for accurate diagnosis, treatment, and healthcare management. The appropriate use of ICD-10 codes not only facilitates effective clinical documentation and reimbursement but also contributes to public health surveillance and research efforts.
As our understanding of myocarditis continues to evolve, ongoing research is critical to identifying new risk factors, improving diagnostic approaches, and developing targeted therapies. By recognizing the signs and symptoms of myocarditis and implementing appropriate management strategies, healthcare providers can significantly improve patient outcomes and reduce the burden of this serious condition.
In conclusion, awareness of the ICD-10 coding for myocardial inflammation is vital for healthcare professionals and patients alike. Accurate coding, combined with early recognition and intervention, can lead to better prognoses and improved quality of life for individuals affected by myocarditis. As we continue to explore the complexities of this condition, we can work towards enhancing cardiovascular health and preventing the complications associated with myocardial inflammation.
Related Topics: