Myocardial inflammation, or myocarditis, is a complex condition characterized by inflammation of the heart muscle, which can lead to significant cardiovascular complications. Understanding the location of myocardial inflammation is crucial for accurate diagnosis, treatment planning, and prognosis. This article will explore the various methods used to determine the location of myocardial inflammation, including clinical presentation, imaging techniques, and histopathological analysis. By providing a comprehensive overview, this article aims to equip healthcare professionals and patients with the knowledge necessary to understand the implications of myocardial inflammation.
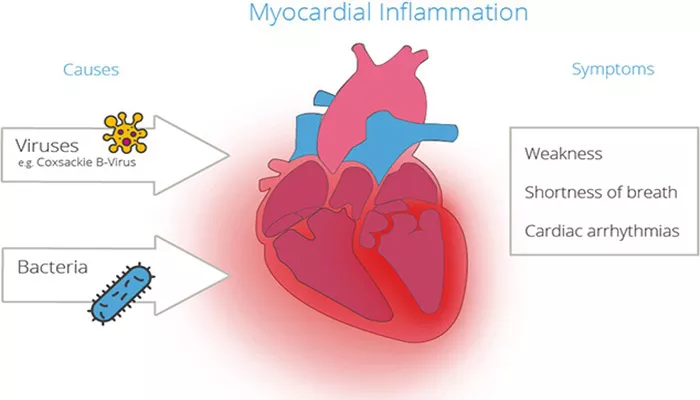
Understanding Myocardial Inflammation
Definition of Myocarditis
Myocarditis is defined as the inflammation of the myocardium, the muscular layer of the heart wall. This condition can result from various etiologies, including viral infections, autoimmune diseases, toxins, and certain medications. The inflammation can lead to structural and functional changes in the heart, which may manifest as arrhythmias, heart failure, or even sudden cardiac death.
Pathophysiology of Myocarditis
The pathophysiology of myocarditis involves a complex interplay between infectious agents, the immune system, and the heart muscle. In many cases, viral infections trigger an immune response that inadvertently damages myocardial cells. This immune-mediated damage can lead to inflammation, necrosis, and fibrosis, ultimately affecting the heart’s ability to function properly.
Importance of Locating Myocardial Inflammation
Determining the location of myocardial inflammation is essential for several reasons:
Diagnosis: Different locations of inflammation may suggest specific underlying causes, guiding diagnostic testing and treatment.
Treatment Planning: The location of inflammation can influence the choice of therapeutic interventions, including medications and lifestyle modifications.
Prognosis: Understanding the extent and location of inflammation can help predict outcomes and potential complications.
Clinical Presentation of Myocarditis
Symptoms of Myocardial Inflammation
The clinical presentation of myocarditis can vary widely, depending on the severity of inflammation and the location within the myocardium. Common symptoms include:
Chest Pain: Often described as sharp or pressure-like, chest pain may indicate inflammation affecting the heart’s pericardium or myocardium.
Shortness of Breath: Patients may experience dyspnea, particularly during exertion or when lying flat, due to impaired cardiac function.
Fatigue: Unexplained fatigue is a common symptom, reflecting reduced cardiac output.
Palpitations: Irregular heartbeats may occur due to inflammation affecting the heart’s electrical conduction system.
Swelling: Peripheral edema or abdominal swelling can result from heart failure secondary to myocarditis.
Physical Examination Findings
During a physical examination, healthcare providers may observe:
Heart Murmurs: Abnormal heart sounds may be detected, indicating valvular involvement or heart failure.
S3 or S4 Gallop: These heart sounds may suggest heart failure or reduced ventricular compliance.
Signs of Heart Failure: Elevated jugular venous pressure, crackles on lung examination, and peripheral edema may indicate fluid overload.
Diagnostic Approaches to Determine the Location of Myocardial Inflammation
Electrocardiogram (ECG)
An electrocardiogram (ECG) is a valuable initial diagnostic tool for assessing myocardial inflammation. It can reveal various changes associated with myocarditis, including:
ST-Segment Changes: Elevation or depression of the ST segment may indicate myocardial injury or ischemia.
T-Wave Abnormalities: Inverted T waves can suggest myocardial inflammation or ischemia.
Arrhythmias: The presence of premature ventricular contractions, atrial fibrillation, or other arrhythmias can indicate electrical instability due to inflammation.
Cardiac Biomarkers
Blood tests measuring cardiac biomarkers are crucial for assessing myocardial inflammation. Key biomarkers include:
Troponin I and T: Elevated levels of troponin indicate myocardial injury and are often seen in patients with myocarditis. The degree of elevation can help assess the extent of inflammation.
B-type Natriuretic Peptide (BNP): Elevated BNP levels suggest heart failure and can provide insights into the severity of cardiac involvement.
Imaging Techniques
Imaging modalities play a pivotal role in determining the location and extent of myocardial inflammation. The most commonly used imaging techniques include:
Echocardiography is a non-invasive imaging technique that uses ultrasound to visualize the heart’s structure and function. Key findings in myocarditis may include:
Left Ventricular Dysfunction: Impaired systolic function can be assessed through measurements of ejection fraction (EF) and wall motion abnormalities.
Regional Wall Motion Abnormalities: Areas of the myocardium may exhibit hypokinesis or akinesis, indicating localized inflammation.
Cardiac Magnetic Resonance Imaging (MRI)
Cardiac MRI is a highly sensitive and specific imaging modality for assessing myocardial inflammation. It provides detailed information about the location and extent of inflammation through various imaging sequences:
Late Gadolinium Enhancement (LGE): This technique highlights areas of myocardial fibrosis or necrosis. In myocarditis, LGE can indicate regions of inflammation and damage.
T1 and T2 Mapping: These advanced techniques can quantify myocardial edema, providing insights into the inflammatory process.
Positron Emission Tomography (PET)
PET imaging can assess myocardial inflammation by evaluating metabolic activity. This technique uses radiotracers to visualize areas of increased glucose metabolism, which may indicate inflammation. PET is particularly useful in cases where myocarditis is suspected but not confirmed by other imaging modalities.
Endomyocardial Biopsy
An endomyocardial biopsy is an invasive procedure that involves obtaining a small sample of heart tissue for histopathological examination. This procedure is typically reserved for cases where the diagnosis is uncertain or when severe myocarditis is suspected. Histological analysis can reveal:
Inflammatory Cell Infiltration: The presence of lymphocytes, macrophages, and other immune cells can indicate active inflammation.
Necrosis and Fibrosis: The extent of myocardial damage can be assessed through tissue analysis, providing insights into the severity of inflammation.
Determining the Location of Myocardial Inflammation
Anterior Myocardial Inflammation
Anterior myocardial inflammation typically affects the anterior wall of the left ventricle and is often associated with ischemic heart disease. Common causes include:
Viral Infections: Certain viral infections can lead to localized inflammation in the anterior myocardium.
Coronary Artery Disease: Ischemia due to coronary artery disease can result in inflammation in the affected region.
Diagnostic Indicators:
ECG Changes: ST-segment elevation in leads V1-V4 may indicate anterior wall involvement.
Echocardiographic Findings: Anterior wall motion abnormalities may be observed on echocardiography.
Inferior Myocardial Inflammation
Inferior myocardial inflammation affects the inferior wall of the left ventricle and is often associated with right coronary artery disease. Common causes include:
Ischemic Events: Myocardial infarction affecting the inferior wall can lead to inflammation.
Viral Infections: Certain viral infections can also affect the inferior myocardium.
Diagnostic Indicators:
ECG Changes: ST-segment elevation in leads II, III, and aVF may suggest inferior wall involvement.
Echocardiographic Findings: Inferior wall motion abnormalities may be evident on echocardiography.
Lateral Myocardial Inflammation
Lateral myocardial inflammation affects the lateral wall of the left ventricle and can be associated with various conditions, including:
Viral Myocarditis: Certain viral infections can lead to inflammation in the lateral myocardium.
Toxic Myocarditis: Exposure to certain toxins may result in localized inflammation.
Diagnostic Indicators:
ECG Changes: ST-segment changes in leads I and aVL may indicate lateral wall involvement.
Echocardiographic Findings: Lateral wall motion abnormalities may be observed on echocardiography.
Global Myocardial Inflammation
Global myocardial inflammation indicates widespread involvement of the myocardium and is often associated with severe forms of myocarditis. Common causes include:
Systemic Infections: Severe viral infections can lead to diffuse myocardial inflammation.
Autoimmune Conditions: Autoimmune diseases can result in generalized inflammation affecting the entire myocardium.
Diagnostic Indicators:
ECG Changes: Diffuse ST-segment changes may be observed.
Echocardiographic Findings: Global left ventricular dysfunction may be evident on echocardiography.
Treatment Options Based on the Location of Myocardial Inflammation
The treatment of myocarditis is largely determined by the underlying cause and the location of inflammation. Key treatment strategies include:
Medical Management
Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be used to reduce inflammation, particularly in autoimmune myocarditis.
Antiviral Therapy: In cases of viral myocarditis, antiviral medications may be considered, although their effectiveness can vary.
Heart Failure Management: Patients with heart failure symptoms may require medications such as ACE inhibitors, beta-blockers, and diuretics to manage fluid overload and improve cardiac function.
Lifestyle Modifications
Dietary Changes: A heart-healthy diet low in saturated fats and sodium can help manage heart failure symptoms and reduce inflammation.
Exercise: Patients should be encouraged to engage in regular physical activity, tailored to their individual tolerance levels.
Cardiac Rehabilitation
Cardiac rehabilitation programs can help patients recover from myocarditis and improve their cardiovascular health. These programs typically include:
Supervised Exercise Training: Gradual increases in physical activity under medical supervision.
Education: Information on heart-healthy living, including diet and stress management.
Surgical Interventions
In severe cases of myocarditis leading to heart failure or life-threatening arrhythmias, surgical interventions may be necessary. Options include:
Implantable Cardioverter-Defibrillator (ICD): Patients at high risk for life-threatening arrhythmias may benefit from ICD implantation.
Heart Transplantation: In cases of severe heart failure unresponsive to medical management, heart transplantation may be considered.
Conclusion
Determining the location of myocardial inflammation is essential for accurate diagnosis, treatment planning, and prognosis in patients with myocarditis. Through a combination of clinical presentation, imaging techniques, and histopathological analysis, healthcare providers can identify the specific areas of inflammation within the myocardium.
Understanding the implications of myocardial inflammation location allows for tailored treatment strategies that can improve patient outcomes. As research continues to evolve in the field of cardiology, ongoing advancements in diagnostic and therapeutic approaches will enhance our ability to manage myocardial inflammation effectively.
Related Topics: