Left ventricular dilation (LVD) refers to the abnormal enlargement and thinning of the heart’s main pumping chamber, the left ventricle. This condition often results from dilated cardiomyopathy (DCM), a disease that impairs the heart muscle’s ability to contract effectively, leading to reduced cardiac output and potential heart failure. Understanding the symptoms, causes, and treatment options for LVD is crucial for timely diagnosis and management.
What Is Left Ventricular Dilation?
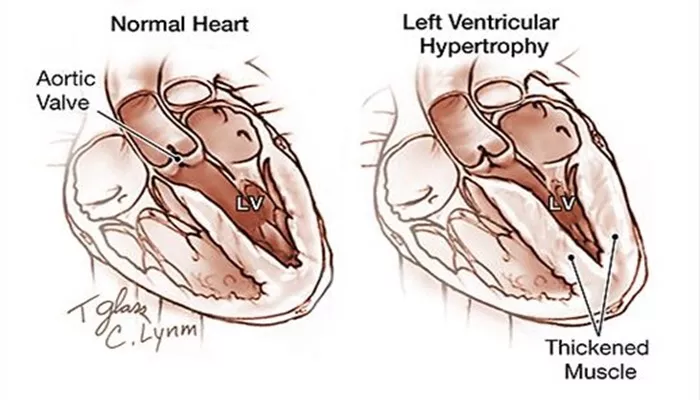
Left ventricular dilation occurs when the left ventricle enlarges and its walls become stretched and thin. This structural change compromises the heart’s ability to pump blood efficiently to the body. LVD is commonly seen in dilated cardiomyopathy, where the heart muscle weakens and dilates, leading to decreased systolic function and heart failure.
Causes of Left Ventricular Dilation
LVD can result from a wide range of underlying conditions that damage or weaken the myocardium (heart muscle). Common causes include:
1. Dilated Cardiomyopathy (DCM)
DCM is the primary cause of LVD, characterized by ventricular enlargement and systolic dysfunction. Causes of DCM include:
Genetic Factors: Familial cardiomyopathies due to inherited gene mutations.
Infections: Viral myocarditis (e.g., Coxsackie B virus), HIV, Lyme disease.
Alcohol Abuse: Chronic excessive alcohol intake leads to alcoholic cardiomyopathy.
Toxins and Drugs: Exposure to heavy metals (lead, mercury, cobalt), certain chemotherapy agents (doxorubicin), and illicit drugs like cocaine and amphetamines.
Autoimmune Diseases: Conditions like polymyositis and sarcoidosis.
Metabolic Disorders: Diabetes, hemochromatosis (iron overload), thyroid disease.
Pregnancy-Related: Peripartum cardiomyopathy occurring late in pregnancy or postpartum.
Coronary Artery Disease: Previous heart attacks causing myocardial damage.
High Blood Pressure: Chronic hypertension increases heart workload leading to dilation.
Heart Valve Disease: Mitral or aortic valve regurgitation causing volume overload.
Arrhythmias: Persistent abnormal heart rhythms can induce dilation.
Nutritional Deficiencies: Thiamine deficiency (beriberi) in rare cases.
2. Other Causes
Chagas Disease: A parasitic infection common in Latin America.
Muscular Dystrophies: Genetic muscle disorders affecting cardiac muscle.
Tachycardia-Induced Cardiomyopathy: Prolonged fast heart rates impair ventricular function.
Symptoms of Left Ventricular Dilation
Symptoms of LVD can be subtle initially and often mimic other cardiovascular or respiratory conditions. They typically develop gradually as the heart’s pumping ability worsens:
Fatigue and Weakness: Due to reduced blood flow to muscles and organs.
Shortness of Breath: Especially during exertion or when lying flat, caused by fluid buildup in the lungs.
Swelling (Edema): Particularly in the legs, ankles, and feet due to fluid retention.
Palpitations: Sensation of rapid, fluttering, or pounding heartbeats caused by arrhythmias.
Chest Pain or Discomfort: May occur during physical activity.
Lightheadedness or Fainting: Resulting from inadequate blood flow or arrhythmias.
Reduced Exercise Tolerance: Difficulty performing physical activities previously tolerated.
In some cases, patients may remain asymptomatic in early stages, making regular cardiovascular evaluation important for those at risk.
Pathophysiology
The dilation of the left ventricle is typically a compensatory response to increased workload or myocardial injury. The stretched ventricular walls lead to decreased contractility (systolic dysfunction), increased wall stress, and eventual heart failure. Over time, this remodeling process worsens cardiac output and promotes arrhythmias, further complicating the clinical course.
Diagnosis
Diagnosis of LVD involves clinical evaluation and imaging studies:
Physical Examination: Detect signs of heart failure such as edema and abnormal heart sounds.
Echocardiography: The primary tool to visualize ventricular size, wall thickness, and function.
Electrocardiogram (ECG): To identify arrhythmias or conduction abnormalities.
Cardiac MRI: Provides detailed myocardial tissue characterization.
Blood Tests: To assess for underlying causes like infections, thyroid function, or iron overload.
Chest X-ray: May show enlarged heart silhouette and pulmonary congestion.
Treatment of Left Ventricular Dilation
The goals of treatment are to reduce symptoms, improve cardiac function, prevent complications, and address underlying causes.
Medical Management
Medications form the cornerstone of therapy for LVD and associated heart failure:
Angiotensin-Converting Enzyme (ACE) Inhibitors and Angiotensin II Receptor Blockers (ARBs): Reduce blood pressure, decrease ventricular remodeling, and improve survival.
Beta-Blockers: Lower heart rate, reduce myocardial oxygen demand, and improve ventricular function.
Mineralocorticoid Receptor Antagonists (MRAs): Help reduce fluid retention and fibrosis.
Diuretics: Remove excess fluid to relieve symptoms of congestion.
Sacubitril/Valsartan (ARNI): Combines ARB with neprilysin inhibition to enhance heart function.
Digoxin: May be used to strengthen contractions and control heart rate.
Ivabradine: Occasionally used to reduce heart rate in heart failure patients.
Anticoagulants: Prevent thromboembolic complications in patients with arrhythmias or severe dysfunction.
Device Therapy
For patients with advanced disease or arrhythmias:
Implantable Cardioverter-Defibrillator (ICD): Monitors and treats life-threatening arrhythmias.
Cardiac Resynchronization Therapy (CRT): Biventricular pacemaker improves coordination of ventricular contractions.
Left Ventricular Assist Device (LVAD): Mechanical pump to support heart function in end-stage cases.
Surgical and Other Interventions
Heart Transplantation: Considered when medical and device therapies fail.
Lifestyle Modifications: Essential adjunct including salt restriction, alcohol cessation, smoking cessation, regular exercise, and managing comorbidities like diabetes and hypertension.
Conclusion
Left ventricular dilation is a serious cardiac condition primarily caused by dilated cardiomyopathy and other factors that impair myocardial function. Recognizing the symptoms early, understanding the diverse causes, and implementing comprehensive treatment strategies are vital to improving patient outcomes. Advances in pharmacologic and device therapies have enhanced the management of LVD, but ongoing research and individualized care remain essential in combating this complex disease.
Related topics: