Obstructive sleep apnea (OSA) is a condition in which the airflow during sleep is repeatedly interrupted due to obstruction in the upper airway. This disruption in breathing can occur multiple times throughout the night, leading to reduced oxygen levels in the blood. Over time, this can strain the cardiovascular system, potentially contributing to the development of pulmonary hypertension (PH), a serious condition where the blood pressure in the pulmonary arteries becomes abnormally high.
The connection between OSA and pulmonary hypertension has been well-documented in clinical studies, as OSA-induced hypoxia (low oxygen levels) and other factors may lead to the development or worsening of PH. In this article, we will explore the mechanisms behind this relationship, the risk factors, diagnostic approaches, and available treatment options for individuals with both conditions.
What is Obstructive Sleep Apnea (OSA)?
Obstructive sleep apnea is a sleep disorder characterized by repeated episodes of partial or complete blockage of the upper airway during sleep. These pauses in breathing can last for several seconds to minutes and can occur hundreds of times throughout the night. This leads to reduced oxygen supply to the body, which triggers an increase in the heart rate and blood pressure. Individuals with OSA often experience daytime fatigue, difficulty concentrating, and an increased risk of cardiovascular diseases.
Mechanisms of OSA
During an OSA event, the muscles in the throat relax excessively, obstructing the airway and preventing proper airflow into the lungs. This leads to a temporary drop in oxygen levels (hypoxia) in the blood. When oxygen levels fall, the body reacts by increasing the production of red blood cells and stimulating the sympathetic nervous system, leading to higher heart rate and blood pressure. These intermittent episodes of hypoxia can have far-reaching effects on the cardiovascular system, including the development of pulmonary hypertension.
Risk Factors for OSA
Several factors increase the risk of developing OSA, including obesity, aging, and anatomical abnormalities in the upper airway. Other risk factors include alcohol use, smoking, and family history. Obesity, in particular, is a significant contributor to OSA, as excess weight can lead to fatty deposits around the neck and throat, increasing the likelihood of airway obstruction during sleep.
What is Pulmonary Hypertension?
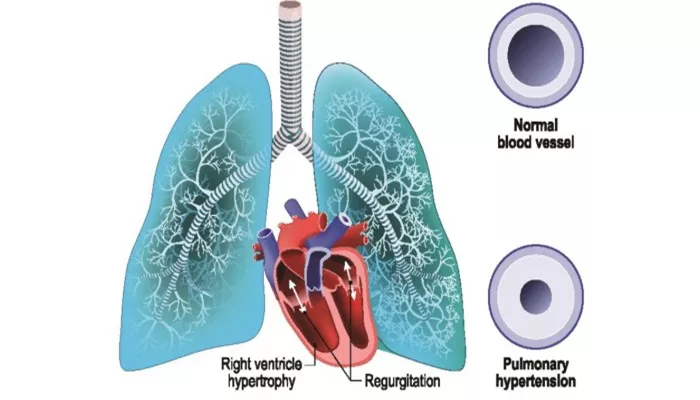
Pulmonary hypertension refers to high blood pressure in the arteries that supply the lungs, which can lead to shortness of breath, fatigue, chest pain, and in severe cases, heart failure. In pulmonary hypertension, the blood vessels in the lungs become narrowed or blocked, making it harder for the heart to pump blood through the lungs, which increases the pressure in these arteries.
Causes of Pulmonary Hypertension
Pulmonary hypertension can result from various causes, including chronic lung diseases, heart conditions, and certain blood clotting disorders. However, one of the lesser-known causes of pulmonary hypertension is obstructive sleep apnea. The continuous strain on the heart and blood vessels due to OSA-induced hypoxia can lead to an increase in pulmonary artery pressure, eventually contributing to the development of pulmonary hypertension.
Symptoms of Pulmonary Hypertension
Symptoms of pulmonary hypertension may vary, but they often include:
- Shortness of breath, especially with physical activity
- Fatigue and weakness
- Chest pain or discomfort
- Swelling in the legs, ankles, or abdomen
- Fainting or dizziness
How Can OSA Lead to Pulmonary Hypertension?
The relationship between OSA and pulmonary hypertension is primarily mediated through episodes of hypoxia (low oxygen levels) that occur during sleep. When the airway becomes obstructed, oxygen levels drop, triggering a cascade of physiological responses that can eventually contribute to pulmonary hypertension.
Hypoxia and the Pulmonary Circulation
During an OSA event, when oxygen levels decrease, the body responds by increasing the production of erythropoietin, a hormone that stimulates the production of red blood cells. In response to chronic low oxygen levels, the blood vessels in the lungs constrict to divert blood flow to areas with better oxygenation. This constriction, known as hypoxic pulmonary vasoconstriction, increases pressure in the pulmonary arteries. Over time, this can lead to the remodeling of these arteries, causing permanent elevation in pulmonary artery pressure—leading to pulmonary hypertension.
Increased Sympathetic Nervous System Activity
Another contributing factor is the activation of the sympathetic nervous system during OSA events. The repeated arousals from sleep due to breathing interruptions result in the release of stress hormones like adrenaline, which increase heart rate and blood pressure. Over time, this constant activation can strain the cardiovascular system, contributing to the development of pulmonary hypertension.
Inflammatory Responses
OSA is also associated with increased systemic inflammation. The intermittent drops in oxygen levels during sleep can cause the release of inflammatory cytokines, which may lead to further damage to the blood vessels in the lungs. Chronic inflammation is a known contributor to the development of pulmonary hypertension.
How Is Pulmonary Hypertension Diagnosed in Patients with OSA?
Diagnosing pulmonary hypertension in patients with OSA can be challenging, as the symptoms of both conditions may overlap. However, several diagnostic tests can help identify pulmonary hypertension in individuals with OSA:
1. Echocardiogram
An echocardiogram is a non-invasive ultrasound test that uses sound waves to create an image of the heart and measure the pressure in the pulmonary arteries. It is one of the most common tests used to diagnose pulmonary hypertension.
2. Right Heart Catheterization
If an echocardiogram suggests pulmonary hypertension, a right heart catheterization may be performed to directly measure the pressures in the pulmonary arteries. This test is considered the gold standard for diagnosing pulmonary hypertension.
3. Polysomnography
Polysomnography is a sleep study that monitors various body functions during sleep, including brain activity, oxygen levels, and heart rate. It is the primary diagnostic tool for identifying obstructive sleep apnea and can help assess the severity of the condition.
Treatment for OSA and Pulmonary Hypertension
Both OSA and pulmonary hypertension are serious conditions, but they can be managed with appropriate treatment. If you have OSA and pulmonary hypertension, your healthcare provider will work with you to create a treatment plan that addresses both conditions simultaneously.
1. Treatment for OSA
The primary treatment for obstructive sleep apnea is the use of a continuous positive airway pressure (CPAP) machine. This device helps keep the airway open during sleep by providing a constant flow of air. Other treatments may include oral appliances or, in severe cases, surgery to remove obstructions from the airway.
2. Treatment for Pulmonary Hypertension
Managing pulmonary hypertension typically involves medications that relax and widen the blood vessels in the lungs, such as endothelin receptor antagonists, phosphodiesterase inhibitors, and prostacyclin analogs. In some cases, oxygen therapy may be recommended to increase oxygen levels in the blood. In severe cases, lung transplantation may be considered.
3. Managing Both Conditions
For individuals with both OSA and pulmonary hypertension, treating the underlying OSA is crucial. By improving oxygenation during sleep, CPAP therapy can help reduce the strain on the heart and pulmonary arteries. Additionally, addressing pulmonary hypertension with medications and lifestyle changes can help improve overall health outcomes.
Conclusion
The relationship between obstructive sleep apnea and pulmonary hypertension highlights the importance of early detection and comprehensive management of both conditions. Individuals with OSA should be regularly monitored for signs of pulmonary hypertension, especially if they experience symptoms such as shortness of breath, fatigue, or chest pain. Early intervention can help prevent the progression of pulmonary hypertension and improve long-term health outcomes. If you suspect that you may have either condition, consult with a healthcare provider to discuss appropriate testing and treatment options.
Related topics: