Metabolic disease represents a spectrum of interconnected disorders, including obesity, insulin resistance, dyslipidemia, and hypertension. Collectively referred to as metabolic syndrome, these conditions significantly elevate the risk of cardiovascular disease, type 2 diabetes, stroke, and chronic kidney disease. The growing prevalence of these disorders globally underscores the importance of effective preventive strategies. Prevention focuses on lifestyle interventions, early risk identification, and regular monitoring. Adopting healthy behaviors not only delays onset but can reverse early metabolic changes. This article presents a comprehensive, evidence-based guide to preventing metabolic disease.
Understanding Metabolic Disease
Metabolic disease encompasses disorders that disrupt normal metabolic processes. The most common form is metabolic syndrome—a cluster of at least three of the following:
- Abdominal obesity
- Elevated fasting glucose
- High triglycerides
- Low HDL cholesterol
- Increased blood pressure
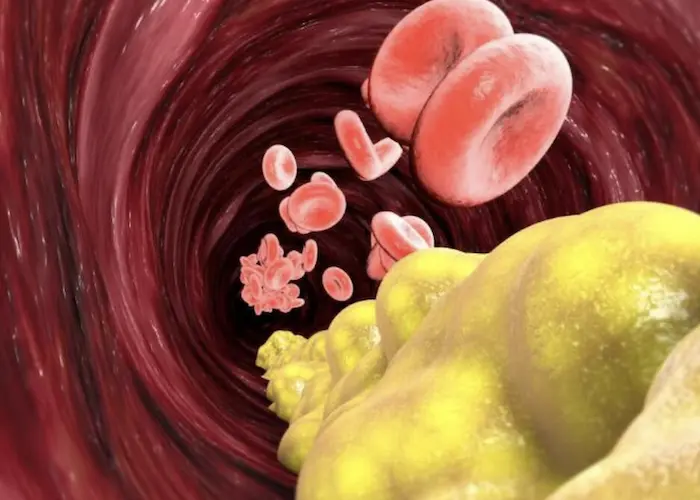
These abnormalities often coexist and potentiate each other’s impact, accelerating atherosclerosis and systemic inflammation.
Causes and Risk Factors
Metabolic disease results from a complex interplay of genetic, behavioral, and environmental factors:
- Poor diet high in processed foods, sugars, and trans fats
- Physical inactivity
- Chronic stress and sleep deprivation
- Excessive alcohol use
- Smoking
- Genetic predisposition
Obesity and insulin resistance are central to most cases.
Key Principles in Prevention
Prioritize Healthy Nutrition
Dietary intervention remains the cornerstone of prevention. A balanced diet should include:
- Whole grains (oats, brown rice, barley)
- High fiber vegetables and fruits
- Lean proteins (fish, poultry, legumes)
- Healthy fats (olive oil, nuts, seeds)
Reduce intake of refined carbohydrates, sugary beverages, processed meats, and trans fats. Moderate sodium consumption aids in blood pressure control. The Mediterranean and DASH diets are supported by strong evidence for metabolic health.
Maintain a Healthy Weight
Weight control is critical. Even modest weight loss (5–10%) improves insulin sensitivity, lipid profiles, and blood pressure. Strategies include:
- Caloric awareness and portion control
- Mindful eating techniques
- Setting realistic weight loss goals
Monitoring body mass index (BMI) and waist circumference helps track progress.
Increase Physical Activity
Regular exercise enhances glucose metabolism, lipid control, and vascular function. Recommendations include:
- At least 150 minutes of moderate aerobic activity weekly
- Strength training twice a week
- Incorporating daily movement: walking, climbing stairs, gardening
Consistency is more important than intensity. Tailor activity to individual capacity.
Optimize Sleep Hygiene
Chronic sleep deprivation disrupts glucose regulation and increases appetite hormones. Prevention includes:
- 7–9 hours of quality sleep per night
- Maintaining a regular sleep-wake schedule
- Reducing screen exposure before bedtime
- Limiting caffeine and alcohol late in the day
Treating sleep apnea or insomnia improves metabolic parameters significantly.
Manage Stress Effectively
Chronic stress activates the hypothalamic-pituitary-adrenal (HPA) axis, raising cortisol and promoting insulin resistance. Interventions:
- Mindfulness-based stress reduction (MBSR)
- Yoga and tai chi
- Deep breathing and progressive muscle relaxation
- Regular physical activity and social engagement
Mental health support reduces emotional eating and sedentary behaviors.
Avoid Harmful Habits
Lifestyle risks include:
- Smoking: Increases insulin resistance and central adiposity
- Excessive alcohol: Raises triglycerides and impairs liver function
Smoking cessation and moderate alcohol consumption (<2 drinks/day for men, <1 drink/day for women) are essential.
Routine Monitoring and Medical Support
Screening Guidelines
Early detection aids prevention. Adults should undergo:
- Fasting glucose or HbA1c every 3 years after age 35
- Lipid panels every 4–6 years or more frequently in high-risk individuals
- Annual blood pressure monitoring
- Waist circumference and BMI tracking
Those with family history or obesity may need earlier screening.
Personalized Risk Assessment
Using tools like the Framingham Risk Score or ASCVD calculator helps stratify cardiovascular risk. Primary care and cardiology teams can guide tailored prevention plans based on risk level.
Role of Medications
For high-risk individuals, medications may be indicated:
- Statins for dyslipidemia
- Metformin for prediabetes with high BMI
- ACE inhibitors or ARBs for hypertension
These do not replace lifestyle changes but complement them.
Special Considerations in At-Risk Groups
Children and Adolescents
The rise in pediatric obesity necessitates early education and intervention. Encourage:
- Home-cooked meals
- Outdoor play over screen time
- Parental modeling of healthy habits
Routine BMI monitoring during pediatric visits is advised.
Women and Metabolic Risk
Pregnancy, menopause, and polycystic ovary syndrome (PCOS) increase metabolic disease risk. Recommendations:
- Gestational diabetes screening during pregnancy
- Regular lipid and glucose checks post-menopause
- Weight and insulin control in PCOS
Hormonal changes require dynamic preventive strategies.
Ethnic Disparities
Certain ethnicities, including South Asians, African Americans, and Hispanics, show higher metabolic risk at lower BMIs.
Early and aggressive prevention, even in the absence of obesity, is critical. Cultural tailoring of dietary and activity plans increases adherence.
Preventing Progression to Diabetes and Heart Disease
The primary goal of metabolic disease prevention is to avoid progression to overt diabetes or cardiovascular events. Intervening early reduces:
- Myocardial infarction
- Stroke
- Chronic kidney disease
Combined lifestyle and pharmacologic interventions offer the best long-term outcomes.
Community and Policy-Level Interventions
Public health approaches support individual changes:
- Clear nutritional labeling
- Taxes on sugary drinks
- Urban planning for walkable spaces
- School programs promoting healthy lunches and physical activity
Prevention succeeds best in supportive environments.
Technology and Digital Tools
Mobile health apps and wearable trackers improve adherence by:
- Monitoring steps and activity
- Logging food intake and weight
- Setting goals and reminders
Digital tools, especially when linked with healthcare providers, enhance outcomes.
Conclusion
Metabolic disease is largely preventable. A proactive approach combining dietary improvements, regular physical activity, stress and sleep management, and routine screenings is essential. Tailoring strategies to individual risk profiles increases adherence and efficacy. Beyond personal responsibility, community and policy changes are needed to support widespread prevention. With coordinated effort, we can curb the rise of metabolic disorders and improve population health.
Related topics: