Pulmonary edema and pulmonary hypertension are two serious conditions that affect the lungs and heart. While each condition has its distinct characteristics, they are often linked in clinical practice, particularly in patients with heart disease. Pulmonary edema refers to the accumulation of fluid in the lungs, which interferes with gas exchange and can lead to severe respiratory distress. Pulmonary hypertension, on the other hand, is a condition characterized by elevated blood pressure in the pulmonary arteries, which can strain the heart and affect circulation to the lungs.
Understanding the relationship between pulmonary edema and pulmonary hypertension is critical for diagnosing and treating patients with these conditions. This article explores how pulmonary edema may lead to or exacerbate pulmonary hypertension, the underlying mechanisms, clinical manifestations, and the available treatment options for these interrelated diseases.
What is Pulmonary Edema?
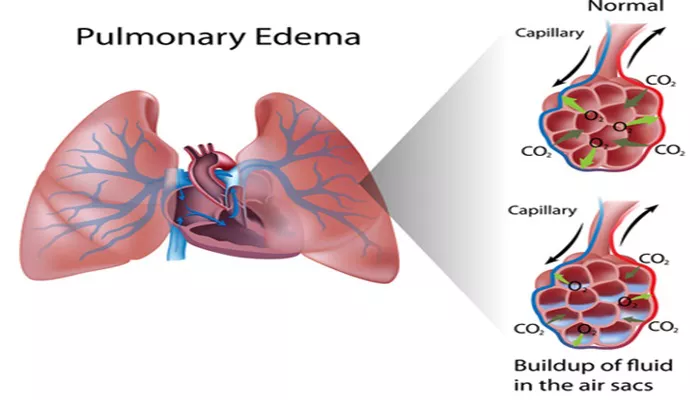
Pulmonary edema is the accumulation of fluid in the lungs, primarily in the alveoli (the tiny air sacs where oxygen exchange occurs). The condition typically results from heart failure, particularly left-sided heart failure, but can also be caused by other factors such as kidney disease, infections, or high altitude exposure. Symptoms of pulmonary edema include shortness of breath, difficulty breathing while lying flat, a feeling of suffocation, and sometimes a frothy pink sputum.
What is Pulmonary Hypertension?
Pulmonary hypertension (PH) is defined by elevated blood pressure within the pulmonary arteries, which are responsible for carrying blood from the heart to the lungs. When these arteries become narrowed or damaged, the heart has to work harder to pump blood through them, leading to increased pressure. Pulmonary hypertension is a progressive disease that can strain the right side of the heart, potentially causing right-sided heart failure if left untreated. Symptoms include shortness of breath, fatigue, chest pain, and dizziness, often worsening with physical activity.
How Pulmonary Edema and Pulmonary Hypertension Are Related
The connection between pulmonary edema and pulmonary hypertension lies in the effects of fluid accumulation in the lungs and its impact on blood flow. When the lungs are flooded with excess fluid due to pulmonary edema, the oxygen exchange process is compromised. This leads to decreased oxygen levels in the blood, which in turn can increase the pressure in the pulmonary arteries as the heart attempts to compensate for the low oxygen state. In chronic cases, this can lead to sustained pulmonary hypertension.
Mechanisms Linking Pulmonary Edema to Pulmonary Hypertension
Several mechanisms can explain how pulmonary edema contributes to the development of pulmonary hypertension:
Increased Blood Volume in the Lungs: Fluid accumulation in the lungs can increase the volume of blood within the pulmonary capillaries, raising the pressure in the pulmonary arteries.
Impaired Gas Exchange: Pulmonary edema reduces the ability of the lungs to exchange oxygen and carbon dioxide efficiently. This can lead to hypoxia (low oxygen levels in the blood), which causes the pulmonary arteries to constrict, raising pulmonary artery pressure.
Left Heart Dysfunction: In many cases, pulmonary edema is caused by left-sided heart failure, which can also lead to pulmonary hypertension. When the left side of the heart is unable to pump blood effectively, blood backs up into the lungs, increasing pulmonary vascular resistance and causing pulmonary hypertension.
Clinical Manifestations of Pulmonary Edema and Pulmonary Hypertension
The clinical signs of both pulmonary edema and pulmonary hypertension overlap in many cases. Patients with pulmonary edema often present with acute or subacute shortness of breath, orthopnea (difficulty breathing while lying flat), and a cough with frothy sputum. Pulmonary hypertension may present with progressive dyspnea, chest pain, and fatigue. The presence of both conditions in the same patient can worsen the severity of symptoms, leading to more complicated clinical presentations.
Diagnosis of Pulmonary Edema and Pulmonary Hypertension
Diagnosing pulmonary edema and pulmonary hypertension involves a combination of patient history, physical examination, imaging studies, and laboratory tests. For pulmonary edema, a chest X-ray or CT scan may show fluid in the lungs. In addition, echocardiography is commonly used to assess heart function, and B-type natriuretic peptide (BNP) levels are often elevated in patients with heart failure-induced pulmonary edema.
Pulmonary hypertension is diagnosed through echocardiography, which estimates pulmonary artery pressure, and confirmed by right heart catheterization, which directly measures the pressure within the pulmonary arteries. Additionally, a CT scan of the chest or pulmonary function tests may be conducted to assess lung function and rule out other causes of increased pulmonary pressure.
Does Pulmonary Edema Cause Pulmonary Hypertension?
While pulmonary edema does not directly “cause” pulmonary hypertension, it can certainly lead to or exacerbate the condition. As fluid accumulates in the lungs and impairs gas exchange, the heart must work harder to pump blood through the pulmonary vasculature. This increased workload can result in elevated pulmonary artery pressure. Furthermore, chronic pulmonary edema due to heart failure can lead to sustained pulmonary hypertension as the heart and lungs continue to struggle to maintain oxygenation and blood flow.
In cases where pulmonary edema is caused by left-sided heart failure, the pressure in the left side of the heart increases, which can cause fluid to back up into the lungs, leading to both pulmonary edema and pulmonary hypertension. The continuous cycle of fluid accumulation and increased pulmonary resistance can create a vicious circle, making it difficult for patients to recover without proper management of both conditions.
Treatment of Pulmonary Edema and Pulmonary Hypertension
The treatment for pulmonary edema and pulmonary hypertension depends on the underlying cause and the severity of the conditions. For pulmonary edema, the primary treatment focuses on removing excess fluid from the lungs and improving heart function. This may involve the use of diuretics, which help the body expel fluid, and medications to improve heart pumping function, such as ACE inhibitors, beta-blockers, or angiotensin II receptor blockers (ARBs).
For pulmonary hypertension, treatment aims to reduce the pressure in the pulmonary arteries and improve heart function.
This can include medications such as phosphodiesterase inhibitors, endothelin receptor antagonists, or prostacyclin analogs. In more severe cases, patients may require oxygen therapy or even surgical interventions, such as atrial septostomy or lung transplantation.
Prevention and Management Strategies
Preventing pulmonary edema and pulmonary hypertension involves managing risk factors such as high blood pressure, heart disease, and chronic lung conditions. Patients with a history of heart failure or other cardiac diseases should work closely with their healthcare provider to manage these conditions and avoid fluid buildup in the lungs. Lifestyle changes, including a heart-healthy diet, regular exercise, and avoiding smoking, can also help prevent the progression of both conditions.
Conclusion
Pulmonary edema and pulmonary hypertension are closely linked conditions, and while pulmonary edema may not directly cause pulmonary hypertension, it can contribute to its development. The interplay between these two conditions, particularly in the context of heart failure, can lead to significant morbidity and complications. Timely diagnosis and appropriate treatment are essential for managing these conditions and improving patient outcomes. By understanding their relationship, clinicians can better address the needs of patients suffering from both pulmonary edema and pulmonary hypertension.
Related topics: