Heart failure (HF) is a condition where the heart is unable to pump blood effectively to meet the body’s needs. As a result, it can lead to various complications, including arrhythmias. In patients with heart failure, pacemakers are used as part of the treatment to manage abnormal heart rhythms and improve the heart’s functionality. Pacemakers provide electrical impulses that can help maintain a regular heart rate and rhythm. The use of a pacemaker can significantly enhance the quality of life in heart failure patients, reducing the symptoms of fatigue, shortness of breath, and dizziness.
Understanding Heart Failure and Its Impact
Heart failure is not a single condition, but rather a complex syndrome that affects the heart’s ability to pump blood. It can occur in several forms, including systolic heart failure, diastolic heart failure, and congestive heart failure. Heart failure may result from a range of conditions, such as coronary artery disease, high blood pressure, or heart valve disease.
As the heart becomes weaker, the electrical signals that regulate its rhythm can also become disrupted, leading to arrhythmias. These irregular heartbeats can further worsen the symptoms of heart failure, making it harder for the heart to pump blood efficiently. To manage these symptoms, a pacemaker is often recommended for patients with heart failure who also suffer from significant arrhythmias.
What is a Pacemaker?
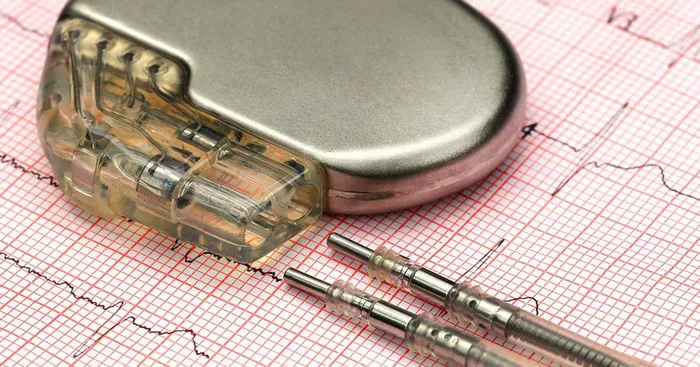
A pacemaker is a small medical device implanted under the skin that helps regulate the heart’s electrical signals. It sends electrical impulses to the heart to correct abnormal heart rhythms. The pacemaker monitors the heart’s rhythm and provides stimulation when the heart’s natural rhythm is too slow or irregular.
Components of a Pacemaker
There are two main components to a pacemaker:
Pulse Generator: This small battery-powered device houses the electrical circuits that control the pacemaker’s function.
Leads: These are thin wires that connect the pulse generator to the heart. The leads deliver electrical impulses to the heart muscle when necessary.
Types of Pacemakers Used for Heart Failure Patients
There are several types of pacemakers, each designed to treat different types of heart rhythm problems. For patients with heart failure, two primary types of pacemakers are often used: traditional single-chamber pacemakers and advanced biventricular pacemakers used in cardiac resynchronization therapy (CRT).
1. Traditional Single-Chamber Pacemaker
A single-chamber pacemaker is typically used to treat patients with bradycardia (slow heart rate). This type of pacemaker is implanted in patients whose heart rhythm is too slow, causing symptoms such as dizziness and fatigue. The pacemaker monitors the heart’s rhythm and sends electrical impulses to stimulate the heart if the rate drops below a certain level.
In heart failure patients, however, a single-chamber pacemaker may not always be effective, especially if the heart’s electrical system is disrupted in more complex ways. As such, this type of pacemaker is less commonly used for heart failure patients with significant electrical abnormalities.
2. Biventricular Pacemaker (Cardiac Resynchronization Therapy)
The biventricular pacemaker, also known as a cardiac resynchronization therapy (CRT) device, is used in patients with heart failure who also have a condition called ventricular dyssynchrony, where the left and right ventricles of the heart beat out of sync. This asynchrony worsens heart function and symptoms of heart failure.
In a CRT system, the pacemaker has three leads: one is placed in the right atrium, one in the right ventricle, and the third in the left ventricle (via a vein in the chest). This setup ensures that both ventricles contract in synchrony, improving the heart’s ability to pump blood. The CRT pacemaker coordinates the contractions of the heart’s ventricles, improving the efficiency of the heart and reducing symptoms such as shortness of breath and fatigue.
Benefits of Biventricular Pacemakers for Heart Failure
For patients with heart failure, the biventricular pacemaker offers several significant benefits:
Improved Heart Function: By synchronizing the heart’s electrical activity, CRT improves the heart’s pumping ability, which leads to better circulation and oxygen delivery to tissues.
Reduced Hospitalizations: Patients who undergo CRT treatment experience fewer hospitalizations due to worsening heart failure symptoms.
Improved Quality of Life: Patients report improved symptoms, greater energy levels, and an enhanced ability to perform daily activities.
Indications for Biventricular Pacemaker Implantation
Not all patients with heart failure are candidates for a biventricular pacemaker. The decision to implant a CRT device is based on several factors, including:
Severe Heart Failure: Typically, patients with NYHA (New York Heart Association) Class III or IV heart failure symptoms are considered candidates for CRT.
Wide QRS Complex: A wide QRS complex on an electrocardiogram (ECG) indicates delayed electrical conduction, which is often seen in patients with ventricular dyssynchrony.
Left Ventricular Ejection Fraction (LVEF): An LVEF of 35% or less is often used as a threshold for CRT candidacy, as patients with low LVEF are more likely to benefit from resynchronization therapy.
How the Pacemaker is Implanted
The implantation of a pacemaker, including a biventricular pacemaker, is generally performed under local anesthesia and mild sedation. The procedure typically takes a few hours and involves the following steps:
Incision: A small incision is made near the collarbone to insert the pacemaker.
Lead Placement: The leads are threaded through blood vessels to the heart. For a biventricular pacemaker, a third lead is placed in the left ventricle via the coronary sinus.
Pacemaker Connection: The leads are connected to the pulse generator, which is implanted just under the skin.
Testing: The device is tested to ensure that it is working properly and that the leads are positioned correctly.
Potential Risks and Complications
While pacemaker implantation is generally safe, there are some potential risks and complications to be aware of:
Infection: As with any surgical procedure, there is a risk of infection at the implant site.
Lead Displacement: The leads may shift after implantation, which may require repositioning.
Device Malfunction: Although rare, the pacemaker may fail to function correctly, leading to complications.
Conclusion
For patients with heart failure, the type of pacemaker used plays a critical role in improving both heart function and quality of life. The biventricular pacemaker, as part of cardiac resynchronization therapy, has proven to be highly effective in treating heart failure with ventricular dyssynchrony. It offers substantial benefits, including improved heart pumping, reduced symptoms, and a decrease in hospitalizations. By synchronizing the contractions of the heart’s ventricles, CRT helps patients manage their heart failure more effectively and live more active lives.
Related Topics: