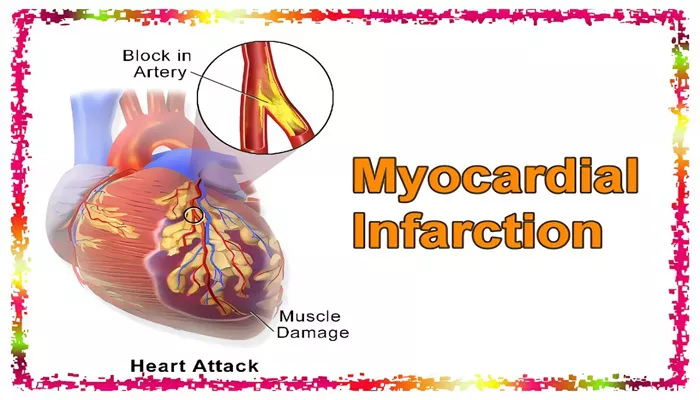
Myocardial infarction (MI), commonly known as a heart attack, is a medical emergency that occurs when the blood flow to a portion of the heart muscle is obstructed, leading to tissue damage. The early detection and diagnosis of myocardial infarction are crucial for effective treatment and improved patient outcomes. One of the most valuable diagnostic tools in this context is the electrocardiogram (ECG), which records the electrical activity of the heart and provides critical information about its function. In this article, we will explore the various ECG changes that indicate myocardial infarction, how they are interpreted, and their clinical significance.
The Importance of ECG in Diagnosing Myocardial Infarction
The ECG is an essential tool in diagnosing myocardial infarction because it can reveal changes in the electrical activity of the heart that occur as a result of ischemia (lack of blood flow) and infarction (tissue death). By analyzing the ECG, healthcare providers can determine the location and extent of the myocardial injury and guide treatment decisions. Early recognition of these changes can help clinicians identify high-risk patients, leading to faster intervention and better outcomes.
ECG changes that suggest myocardial infarction may be subtle or pronounced, and they depend on factors such as the type of infarction (e.g., STEMI vs. NSTEMI), the stage of the infarction, and the area of the heart affected. This makes it critical to understand the various types of changes and how they correlate with the clinical scenario.
Key ECG Changes Indicating Myocardial Infarction
Several ECG changes can indicate that a patient is experiencing or has experienced a myocardial infarction. These changes include alterations in the P wave, the QRS complex, the T wave, and the ST segment. The most common and significant changes are found in the ST segment, which is why these changes are often referred to as “ST elevation” or “ST depression” in the context of myocardial infarction.
1. ST Segment Elevation
ST segment elevation is one of the hallmark ECG findings in a STEMI (ST-segment elevation myocardial infarction), a type of heart attack where there is a complete blockage of a coronary artery. When the blood supply to the heart muscle is completely blocked, the affected tissue becomes ischemic, leading to an upward deflection in the ST segment of the ECG.
In a normal ECG, the ST segment is flat, representing the period when the ventricles are in a resting state after contraction. In a myocardial infarction, the ischemic tissue generates abnormal electrical activity, causing the ST segment to elevate above the baseline.
Key points about ST segment elevation include:
The elevation is typically seen in two or more contiguous leads (i.e., leads that are anatomically adjacent on the ECG). The specific leads affected will help identify the region of the heart that is undergoing infarction.
ST elevation is most often associated with a STEMI, which is a more severe type of heart attack and requires immediate intervention, such as percutaneous coronary intervention (PCI) or fibrinolytic therapy.
ST segment elevation is typically seen within minutes to hours of the onset of symptoms and can persist for several hours after the infarction.
2. ST Segment Depression
ST segment depression is a key ECG change associated with non-ST-elevation myocardial infarction (NSTEMI), a type of heart attack in which there is partial blockage or narrowing of the coronary artery, leading to ischemia without complete occlusion. Unlike STEMI, NSTEMI does not cause significant ST segment elevation, but it often results in ST segment depression.
ST segment depression is often seen as a downward deflection of the ST segment, typically occurring in the leads that are distant from the site of ischemia. The depression is usually less pronounced than in STEMI but can still be clinically significant.
Key points about ST segment depression include:
ST depression can occur in multiple leads, particularly the lateral or inferior leads, depending on the location of the ischemia.
It is a common finding in NSTEMI and can be seen alongside other signs, such as T wave inversions.
ST segment depression is generally less specific than ST elevation and may be seen in a variety of other conditions, including angina, pericarditis, and electrolyte imbalances.
3. T Wave Inversions
T wave inversions are another significant ECG change that can occur in myocardial infarction, particularly in the later stages after the initial ischemic event. The T wave normally represents the repolarization (relaxation) of the ventricles, and its inversion can indicate myocardial injury or ischemia.
During a myocardial infarction, the affected area of the heart may experience a delayed repolarization, leading to an inversion of the T wave. T wave inversions can occur in the leads that are affected by the infarction and may persist for several days or weeks after the initial event.
Key points about T wave inversions include:
T wave inversions can be seen in both STEMI and NSTEMI, although they are more commonly associated with NSTEMI or subendocardial infarctions.
The presence of T wave inversions in specific leads can help identify the location of the myocardial injury.
T wave inversions may be transient and may resolve over time as the infarcted tissue heals.
4. Pathological Q Waves
Pathological Q waves are often considered a sign of irreversible myocardial damage and are seen in the later stages of myocardial infarction, particularly after the tissue has undergone necrosis. A Q wave is a small downward deflection at the beginning of the QRS complex, and in a normal ECG, it is usually not prominent or may even be absent in many leads.
However, when there is a significant amount of myocardial tissue death, the electrical activity from the affected area results in the appearance of deep and wide Q waves, indicating that the myocardial tissue is no longer viable.
Key points about pathological Q waves include:
Pathological Q waves are usually seen several hours to days after the onset of the infarction and persist long after the acute phase of the event.
These Q waves are typically seen in the leads that correspond to the affected region of the heart (e.g., anterior leads for an anterior wall infarction).
The presence of pathological Q waves suggests that a significant portion of the heart muscle has been irreversibly damaged and that the patient may be at higher risk for complications such as heart failure.
ECG Findings and Myocardial Infarction Location
The ECG changes seen in myocardial infarction can provide important clues about the location of the infarction. The location of ST elevation, depression, T wave inversions, and Q waves can help clinicians determine which part of the heart is affected. Common locations of infarction and their corresponding ECG findings include:
1. Anterior Wall Myocardial Infarction
Anterior wall infarctions are commonly associated with blockage in the left anterior descending (LAD) coronary artery. ECG changes typically include:
- ST elevation in the precordial leads (V1-V4)
- Pathological Q waves in the same leads
2. Inferior Wall Myocardial Infarction
Inferior wall infarctions are often caused by blockage of the right coronary artery or the left circumflex artery. ECG findings typically include:
- ST elevation in the inferior leads (II, III, aVF)
- Pathological Q waves in the same leads
3. Lateral Wall Myocardial Infarction
Lateral wall infarctions are associated with blockage of the left circumflex artery. ECG changes include:
- ST elevation in the lateral leads (I, aVL, V5, V6)
- Possible T wave inversions or pathological Q waves in these leads
Conclusion
In conclusion, the ECG is a powerful diagnostic tool that plays a crucial role in identifying myocardial infarction. By analyzing changes in the ST segment, T waves, and Q waves, healthcare providers can determine the location and severity of the infarction, which is critical for guiding treatment decisions. Prompt recognition of ECG changes associated with myocardial infarction can significantly improve patient outcomes by enabling early intervention, such as reperfusion therapy or the use of medications to restore blood flow to the heart.
Related topics: