Heart function is a crucial aspect of overall health. When the heart’s function drops to as low as 15%, it signals severe heart failure, a condition that significantly impacts life expectancy. However, how long you can live with only 15% heart function depends on many factors, such as the underlying cause, available treatments, and lifestyle changes. In this article, we explore what it means to have 15% heart function, the prognosis for those with this condition, and how to manage it effectively for a better quality of life.
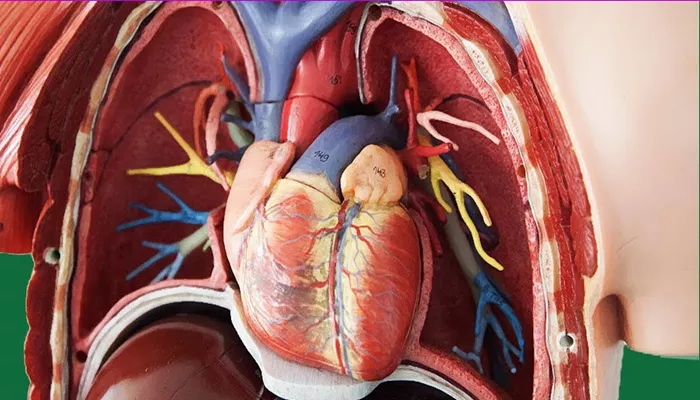
What Does 15% Heart Function Mean?
Heart function is typically measured using a metric known as the ejection fraction (EF). This is the percentage of blood pumped out of the heart with each beat. A normal EF ranges from 50% to 70%. When the EF falls below 40%, it is indicative of heart failure. With an EF as low as 15%, the heart is only pumping out 15% of the blood in each beat, which is severely inadequate for sustaining normal bodily functions.
Understanding Heart Failure
Heart failure occurs when the heart is unable to pump blood efficiently to meet the body’s demands. In cases where the heart’s function drops to 15%, this condition is often referred to as end-stage heart failure. This stage is considered critical, and without proper management, it can lead to severe complications or death.
Causes of Severe Heart Failure
The causes of severe heart failure can vary. Common underlying conditions include coronary artery disease, high blood pressure, heart valve disease, and cardiomyopathy. In some cases, a heart attack or damage to the heart muscle can result in significant reduction in heart function.
Prognosis and Life Expectancy with 15% Heart Function
The prognosis for someone with 15% heart function depends on several factors, including the underlying cause of the heart failure, the individual’s age, overall health, and response to treatment. While it is impossible to predict exactly how long someone will live with 15% heart function, there are some general guidelines based on research and clinical experience.
Survival Rates in Severe Heart Failure
Studies have shown that individuals with heart failure and a very low ejection fraction, such as 15%, have a significantly lower life expectancy compared to those with higher heart function. According to data, the survival rate for patients with end-stage heart failure can range from one to five years, depending on treatment and overall health. However, these numbers can vary widely from patient to patient.
How Treatments Impact Life Expectancy
Advances in medical treatments for heart failure have improved the outlook for many patients with severely reduced heart function. Medications like ACE inhibitors, beta-blockers, and diuretics can help manage symptoms and improve heart function. In some cases, heart transplant surgery or the implantation of a left ventricular assist device (LVAD) may be necessary to support the heart and extend life expectancy.
Managing 15% Heart Function: Treatment Options
While 15% heart function is extremely low, there are various treatment options that can help improve quality of life and potentially extend life expectancy. The primary goal of treatment is to reduce symptoms, prevent complications, and improve heart function as much as possible.
Medications for Heart Failure
Several classes of medications are used to manage heart failure and improve heart function. These include:
- ACE inhibitors: Help relax blood vessels and improve blood flow
- Beta-blockers: Reduce the heart’s workload and help control heart rate
- Diuretics: Help reduce fluid buildup in the body
- Digoxin: Helps strengthen heart contractions and improves symptoms
These medications are typically prescribed in combination to manage heart failure symptoms and slow down the progression of the disease.
Heart Transplant and LVAD
In cases where medications and lifestyle changes are insufficient, more invasive treatments may be needed. A heart transplant is often considered for patients with end-stage heart failure who are otherwise healthy enough to undergo surgery. The LVAD is a mechanical pump that helps the heart pump blood and is often used as a bridge to a heart transplant for patients who are not candidates for immediate surgery.
Lifestyle Changes to Improve Heart Function
In addition to medical treatments, lifestyle changes are essential for managing heart failure and improving quality of life. For patients with 15% heart function, these changes can make a significant difference in symptom management and overall well-being.
Diet and Nutrition
A heart-healthy diet is crucial for individuals with heart failure. Reducing sodium intake can help control fluid retention, while eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall cardiovascular health. Omega-3 fatty acids, found in fish and certain supplements, are also beneficial for heart health.
Physical Activity and Exercise
Although physical activity must be carefully managed in cases of severe heart failure, regular exercise can help strengthen the heart and improve circulation. A doctor or physical therapist will work with patients to develop a safe exercise plan tailored to their specific needs.
Stress Management
Chronic stress can exacerbate heart failure symptoms. Practicing stress-reduction techniques such as deep breathing, meditation, or yoga can improve mental well-being and reduce the strain on the heart.
Complications and Monitoring
Patients with 15% heart function are at high risk for complications such as arrhythmias (irregular heartbeats), blood clots, kidney problems, and liver damage. Regular monitoring and follow-up appointments with a healthcare provider are essential to manage these risks effectively.
Arrhythmias and Sudden Cardiac Arrest
One of the most serious risks for individuals with severely reduced heart function is the development of arrhythmias, which can lead to sudden cardiac arrest. Patients may be fitted with an implantable cardioverter-defibrillator (ICD) to monitor for life-threatening arrhythmias and deliver shocks if necessary to restore normal heart rhythm.
Kidney and Liver Damage
Heart failure can lead to poor circulation, which can affect the kidneys and liver. This can result in further complications, such as fluid retention, electrolyte imbalances, and organ failure. Monitoring kidney and liver function through regular blood tests is essential for individuals with 15% heart function.
Conclusion
Living with 15% heart function is challenging, but with the right medical treatment and lifestyle adjustments, it is possible to manage symptoms and extend life expectancy. The key to surviving with severely reduced heart function is early diagnosis, appropriate medical intervention, and ongoing monitoring. With advances in heart failure treatments and a proactive approach to managing the condition, many patients with 15% heart function can live meaningful and fulfilling lives for several years.
Related topics: