Pulmonary hypertension (PH) is a condition characterized by high blood pressure in the arteries that supply the lungs, which can result in significant cardiovascular complications. Among the potential complications of PH, syncope—or fainting—is a concerning and common symptom. Syncope occurs when there is a temporary loss of consciousness due to insufficient blood flow to the brain. Understanding why pulmonary hypertension leads to syncope is crucial for the proper management of affected individuals. In this article, we will explore the underlying mechanisms, contributing factors, and treatment options related to the relationship between pulmonary hypertension and syncope.
What is Pulmonary Hypertension?
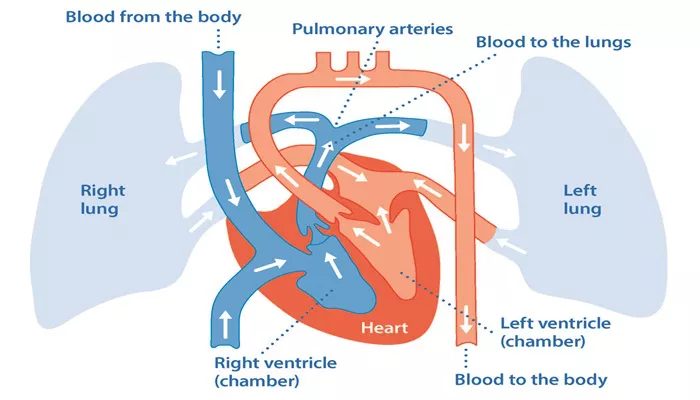
Pulmonary hypertension (PH) refers to high blood pressure in the arteries that carry blood from the heart to the lungs. This condition occurs when these arteries become narrowed or blocked, leading to increased resistance to blood flow. The heart, specifically the right ventricle, has to work harder to pump blood through the lungs. Over time, this increased strain can lead to right-sided heart failure and other complications.
Types of Pulmonary Hypertension
There are several different types of pulmonary hypertension, including:
Primary pulmonary hypertension (idiopathic PH), where the cause is unknown.
Secondary pulmonary hypertension, which results from other conditions such as left heart disease, lung diseases (like chronic obstructive pulmonary disease or pulmonary fibrosis), or blood clots in the lungs.
Pulmonary arterial hypertension (PAH), a specific type of PH that primarily affects the arteries of the lungs.
Symptoms of Pulmonary Hypertension
Common symptoms of pulmonary hypertension include:
- Shortness of breath, particularly during physical activity.
- Fatigue and weakness.
- Chest pain or discomfort.
- Swelling in the legs, ankles, or abdomen.
- Fainting episodes (syncope).
What is Syncope?
Syncope is the medical term for fainting or temporary loss of consciousness. It occurs when there is insufficient blood flow to the brain, often due to a sudden drop in blood pressure or impaired heart function. Syncope can be caused by a variety of factors, including dehydration, standing up too quickly, or underlying cardiovascular conditions. In patients with pulmonary hypertension, syncope is often a result of the strain that PH places on the heart and blood vessels.
Symptoms of Syncope
Common symptoms of syncope include:
Dizziness or lightheadedness before fainting.
Blurred vision or “seeing stars.”
Nausea or a feeling of weakness.
Loss of consciousness, followed by a quick recovery once lying down or with medical intervention.
Why Does Pulmonary Hypertension Cause Syncope?
The relationship between pulmonary hypertension and syncope is complex and stems from several factors related to the impaired function of the heart and circulatory system in PH patients. Below, we will explore the key mechanisms that contribute to syncope in individuals with pulmonary hypertension.
1. Impaired Right Ventricular Function
In pulmonary hypertension, the right side of the heart, which is responsible for pumping blood to the lungs, becomes strained due to the increased pressure in the pulmonary arteries. Over time, this strain can cause the right ventricle to enlarge and weaken, reducing its ability to pump blood effectively. As the right ventricle fails to pump enough blood to the lungs, blood flow to the heart and brain can decrease, leading to fainting episodes. This is especially true during physical activity or other situations that increase the demand for blood flow.
2. Low Cardiac Output
As pulmonary hypertension progresses, the heart’s ability to pump blood effectively diminishes, resulting in a decrease in cardiac output. Cardiac output refers to the amount of blood the heart pumps per minute, and it is critical for maintaining proper blood flow to vital organs, including the brain. In individuals with PH, low cardiac output due to right heart failure can cause insufficient perfusion of the brain, leading to syncope. This is more likely to occur during exertion or when the body demands more oxygenated blood.
3. Hypoxia (Low Oxygen Levels)
Pulmonary hypertension can also result in hypoxia, or low oxygen levels in the blood, because the lungs are not able to efficiently exchange oxygen due to the increased pressure in the pulmonary arteries. Hypoxia places additional strain on the cardiovascular system, and if the brain does not receive adequate oxygen, syncope can occur. In severe cases, episodes of hypoxia during sleep or physical activity can trigger fainting spells, especially in individuals with poorly controlled PH.
4. Vasodilation and Blood Pooling
In some individuals with pulmonary hypertension, medications or the body’s natural compensatory mechanisms can lead to vasodilation, or the widening of blood vessels. While vasodilation is a normal response to low blood pressure or inadequate blood flow, it can sometimes exacerbate the problem by causing blood to pool in the extremities, further reducing the amount of blood flowing to the brain. This can trigger syncope in patients with pulmonary hypertension, especially in the presence of other factors like dehydration or blood volume changes.
5. Arrhythmias (Abnormal Heart Rhythms)
Another contributing factor to syncope in patients with pulmonary hypertension is the increased risk of arrhythmias. The strain on the heart due to pulmonary hypertension can lead to electrical disturbances in the heart, causing abnormal heart rhythms. These arrhythmias can reduce the heart’s ability to pump blood effectively, leading to a sudden drop in blood pressure and subsequent loss of consciousness. The occurrence of arrhythmias in PH patients is a serious concern and often requires urgent medical attention.
Risk Factors for Syncope in Pulmonary Hypertension
Several factors can increase the likelihood of syncope in individuals with pulmonary hypertension. These include:
Severe PH: The more advanced the pulmonary hypertension, the greater the likelihood of syncope, particularly if right heart failure is present.
Physical activity: Exercise or any form of exertion increases the heart’s demand for oxygenated blood. In PH patients, the heart may not be able to meet these demands, leading to fainting episodes.
Medications: Some medications used to treat pulmonary hypertension, such as vasodilators, can lower blood pressure and increase the risk of syncope.
Comorbid conditions: Patients with other cardiovascular diseases, such as coronary artery disease or heart failure, are at an increased risk of syncope due to the additional strain on the heart.
Dehydration or blood loss: Reduced blood volume can exacerbate syncope by lowering blood pressure, making it more difficult for the heart to pump blood effectively.
Diagnosing Syncope in Pulmonary Hypertension
Diagnosing syncope in patients with pulmonary hypertension requires a thorough evaluation of both the cardiovascular system and the underlying cause of the fainting episodes. Some common diagnostic tests include:
1. Electrocardiogram (ECG)
An electrocardiogram records the electrical activity of the heart and can help identify arrhythmias or other abnormal heart rhythms that may contribute to syncope.
2. Echocardiogram
An echocardiogram uses ultrasound waves to create an image of the heart and measure its function, including the ability of the right ventricle to pump blood. This test can help identify the severity of pulmonary hypertension and assess the right heart’s function.
3. Tilt Table Test
A tilt table test is used to evaluate how the body’s blood pressure responds to changes in position. This test can help identify the causes of syncope, including orthostatic hypotension or vasovagal syncope.
4. Right Heart Catheterization
Right heart catheterization is the gold standard for diagnosing pulmonary hypertension. It measures the pressures in the pulmonary arteries and assesses the overall function of the right heart.
Treatment Options for Pulmonary Hypertension and Syncope
Managing syncope in patients with pulmonary hypertension requires addressing the underlying causes of both conditions.
Treatment options may include:
1. Medications
Medications used to treat pulmonary hypertension, such as endothelin receptor antagonists, phosphodiesterase inhibitors, and prostacyclin analogs, can help reduce the pressure in the pulmonary arteries and improve heart function. These medications may reduce the risk of syncope by improving blood flow and oxygenation.
2. Oxygen Therapy
For patients with hypoxia-related syncope, supplemental oxygen therapy may be recommended to ensure adequate oxygen levels in the blood, especially during physical activity or sleep.
3. Lifestyle Modifications
Patients with pulmonary hypertension are encouraged to avoid excessive physical exertion and to take measures to avoid dehydration. Salt and fluid intake may be adjusted to help manage blood pressure and prevent fainting episodes.
4. Heart-Related Treatments
If arrhythmias are contributing to syncope, medications or interventions such as a pacemaker may be required to regulate heart rhythms and prevent fainting episodes.
Conclusion
Syncope is a common and concerning symptom of pulmonary hypertension. Understanding the underlying mechanisms that link PH with fainting is essential for proper diagnosis and treatment. Early detection and appropriate management of both pulmonary hypertension and syncope can significantly improve quality of life and prevent complications. If you or someone you know experiences fainting episodes, it is crucial to consult a healthcare provider for a thorough evaluation and tailored treatment plan.
Related topics: