An anterior myocardial infarction (AMI) refers to a heart attack that occurs in the front part of the heart, specifically the anterior wall of the left ventricle. This type of heart attack is typically caused by the blockage of one or more coronary arteries that supply blood to this region. AMI can lead to significant damage to the heart muscle, affecting its ability to pump blood efficiently. Understanding the causes of anterior myocardial infarction is essential for prevention, early diagnosis, and effective treatment. In this article, we will delve into the factors that contribute to anterior MI, how it occurs, and the steps individuals can take to reduce the risk of experiencing it.
What is Anterior Myocardial Infarction?
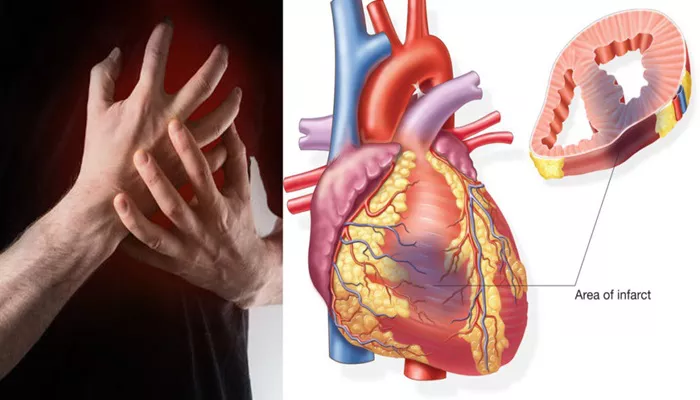
Anterior myocardial infarction occurs when blood flow to the front portion of the heart is blocked. This blockage usually involves one of the main coronary arteries, specifically the left anterior descending (LAD) artery, which is responsible for supplying oxygen-rich blood to the anterior wall of the left ventricle. A blockage in the LAD artery can cause severe damage to the heart muscle, leading to complications such as heart failure, arrhythmias, and even death if not treated promptly.
Location of the Infarction
The location of the infarction—on the anterior wall of the left ventricle—plays a significant role in the severity of the heart attack. This region is critical for the pumping function of the heart, and any damage to it can severely impact the heart’s ability to deliver oxygenated blood throughout the body.
Symptoms of Anterior Myocardial Infarction
Common symptoms of anterior myocardial infarction include:
- Chest pain or discomfort, often described as pressure or tightness.
- Shortness of breath or difficulty breathing.
- Fatigue or weakness.
- Lightheadedness or fainting.
- Pain in the arm, back, jaw, neck, or stomach.
Causes of Anterior Myocardial Infarction
The primary cause of anterior myocardial infarction is the blockage of the coronary arteries, specifically the left anterior descending artery. This blockage typically occurs due to atherosclerosis, a condition where fatty deposits, known as plaques, build up within the arteries. However, other factors can contribute to the development of an anterior MI. Below, we explore the various causes and risk factors associated with this condition.
Atherosclerosis: The Primary Cause
Atherosclerosis is the most common underlying cause of anterior myocardial infarction. It involves the gradual buildup of cholesterol, fatty substances, and other materials in the walls of the coronary arteries. Over time, these deposits form plaques that narrow and harden the arteries, restricting blood flow. If a plaque ruptures, a blood clot can form, completely obstructing the artery and leading to a heart attack.
Coronary Artery Spasm
In some cases, an anterior myocardial infarction can be caused by a coronary artery spasm. A spasm is a temporary constriction of the artery, which reduces blood flow. These spasms can be triggered by factors such as stress, drug use (e.g., cocaine), or cold temperatures. While coronary artery spasms are less common than atherosclerosis, they can still lead to significant heart damage if they result in a prolonged reduction in blood supply.
Embolism or Blood Clots
An embolism occurs when a clot or other material, such as fat or air, travels through the bloodstream and becomes lodged in a coronary artery, blocking blood flow. This can lead to a heart attack, including anterior MI. Although embolism-related heart attacks are less common, they are a known risk factor, particularly in individuals with certain conditions, such as atrial fibrillation or after heart surgery.
Risk Factors for Anterior Myocardial Infarction
Certain lifestyle factors, conditions, and genetic predispositions increase the risk of developing anterior myocardial infarction. The following risk factors are commonly associated with this type of heart attack:
1. High Blood Pressure
Hypertension, or high blood pressure, is a leading risk factor for myocardial infarction. High blood pressure can damage the walls of the coronary arteries over time, making them more prone to atherosclerosis and plaque buildup. Additionally, hypertension places extra strain on the heart, increasing the likelihood of a heart attack.
2. High Cholesterol Levels
Elevated cholesterol levels, particularly low-density lipoprotein (LDL) or “bad” cholesterol, contribute to the development of atherosclerosis. High levels of LDL cholesterol promote the buildup of fatty plaques in the arteries, increasing the risk of a blockage that could lead to an anterior myocardial infarction.
3. Smoking
Smoking is a major contributor to cardiovascular disease and increases the risk of heart attacks. Smoking damages the blood vessels, promotes clot formation, and accelerates the development of atherosclerosis. Smokers are more likely to experience anterior MI compared to nonsmokers.
4. Diabetes
Diabetes increases the risk of atherosclerosis due to the damaging effects of high blood sugar levels on the blood vessels. Individuals with diabetes are more likely to develop coronary artery disease, which can lead to anterior myocardial infarction. Poorly controlled blood sugar levels further exacerbate this risk.
5. Family History of Heart Disease
A family history of heart disease, particularly coronary artery disease, can increase an individual’s risk of developing an anterior myocardial infarction. Genetic factors can influence the development of atherosclerosis, making those with a family history more susceptible to heart attacks.
6. Obesity
Obesity is associated with several risk factors for heart disease, including high blood pressure, high cholesterol, and diabetes. Excess weight puts additional strain on the heart, increasing the likelihood of cardiovascular events such as anterior myocardial infarction.
7. Physical Inactivity
Lack of physical activity is a significant risk factor for heart disease. Regular exercise helps maintain healthy cholesterol levels, blood pressure, and weight, all of which are important for preventing heart attacks. Sedentary lifestyles contribute to the development of conditions like obesity and hypertension, which in turn increase the risk of anterior MI.
Symptoms and Diagnosis of Anterior Myocardial Infarction
The symptoms of anterior myocardial infarction are similar to those of other types of heart attacks but can be more severe due to the location of the infarction. Timely recognition and diagnosis are critical to prevent long-term damage to the heart muscle.
Symptoms of Anterior Myocardial Infarction
Patients with anterior MI often experience the following symptoms:
- Severe chest pain or discomfort, often described as tightness, pressure, or a crushing sensation.
- Pain radiating to the left arm, jaw, back, or neck.
- Shortness of breath, especially during physical activity or at rest.
- Lightheadedness, dizziness, or fainting.
- Cold sweat and nausea.
Diagnostic Methods
Several diagnostic tests are used to confirm the presence of anterior myocardial infarction and determine the extent of heart damage:
Electrocardiogram (ECG): An ECG records the electrical activity of the heart and can detect abnormalities indicative of a heart attack.
Blood Tests: Blood tests are used to measure levels of cardiac enzymes, such as troponin, which are elevated in the blood after a heart attack.
Echocardiogram: This imaging test provides a visual of the heart’s structure and function, helping to assess the damage caused by a myocardial infarction.
Coronary Angiography: Coronary angiography involves injecting a dye into the coronary arteries to identify blockages or narrowing of the arteries.
Treatment of Anterior Myocardial Infarction
The treatment for anterior myocardial infarction aims to restore blood flow to the affected region of the heart and prevent further damage. The primary goal is to minimize the risk of complications and improve long-term outcomes.
1. Medications
Medications are used to manage symptoms and prevent further heart damage. Common medications include:
Antiplatelet drugs (e.g., aspirin) to prevent blood clot formation.
Thrombolytic drugs to dissolve blood clots and restore blood flow.
Beta-blockers to reduce the heart’s workload and prevent arrhythmias.
ACE inhibitors or angiotensin receptor blockers (ARBs) to lower blood pressure and reduce strain on the heart.
2. Percutaneous Coronary Intervention (PCI)
PCI, also known as angioplasty, involves using a catheter to open blocked arteries. A stent may be placed to keep the artery open, restoring blood flow to the heart.
3. Coronary Artery Bypass Grafting (CABG)
In severe cases, when PCI is not an option or the blockage is too extensive, coronary artery bypass grafting (CABG) surgery may be required. This surgery involves creating new pathways for blood to flow to the heart by bypassing blocked arteries.
Conclusion
Anterior myocardial infarction is a serious condition that requires immediate medical intervention. Understanding the causes and risk factors of anterior MI can help in its prevention and early diagnosis. By addressing modifiable risk factors such as high blood pressure, high cholesterol, smoking, and diabetes, individuals can significantly reduce their chances of experiencing a heart attack. Early diagnosis and timely treatment are critical to improving outcomes for patients with anterior myocardial infarction.
Related topics: