Coronary artery calcification (CAC) refers to the buildup of calcium deposits in the coronary arteries, which supply blood to the heart muscle. This condition is often an indicator of coronary artery disease (CAD), a leading cause of heart attacks and other cardiovascular complications. While the presence of any coronary artery calcification is concerning, the severity of the condition varies depending on the extent of the calcification.
Moderate coronary artery calcification is typically diagnosed through imaging tests such as a coronary calcium scan (or CT scan), which quantifies the amount of calcium present in the coronary arteries. The level of calcification can be classified into different categories—none, mild, moderate, and severe. Moderate CAC signifies a moderate degree of plaque buildup, which can increase the risk of cardiovascular events, such as heart attack and stroke. Understanding how serious this condition can be is crucial for appropriate management and risk reduction.
What Is Moderate Coronary Artery Calcification?
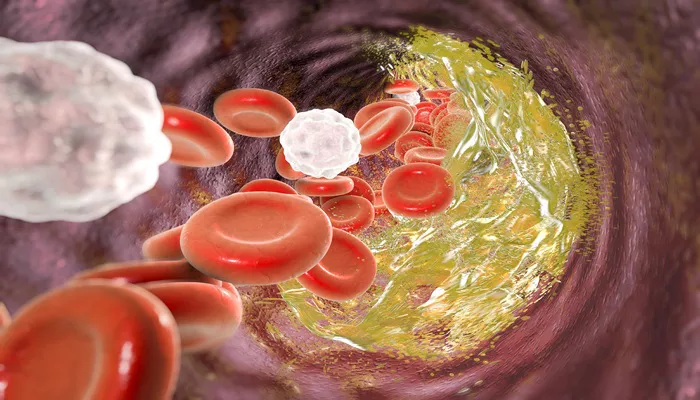
Moderate coronary artery calcification indicates that there is a moderate amount of calcium buildup in the coronary arteries. This calcification is a marker of atherosclerosis, the process in which plaque (composed of fat, cholesterol, and other substances) builds up in the walls of the arteries. Over time, the plaque hardens due to the deposition of calcium, making the arteries stiffer and narrower.
The presence of moderate calcification suggests that there may be significant underlying atherosclerotic plaque, which can partially obstruct blood flow to the heart muscle. This reduction in blood flow can lead to ischemia (insufficient oxygen supply) and increase the risk of adverse cardiovascular events.
Why Does Coronary Artery Calcification Matter?
Calcium deposits in the arteries occur as part of the body’s natural response to injury or inflammation. In the case of coronary artery disease, the arteries become damaged due to factors like high cholesterol, high blood pressure, smoking, or diabetes. The body’s immune response leads to the formation of plaque, which may eventually calcify.
Coronary artery calcification serves as a warning sign that atherosclerosis is present and progressing. The more calcium there is in the arteries, the more likely it is that significant plaque buildup has occurred, which increases the risk of a heart attack or other cardiovascular events. The amount of calcification directly correlates with the severity of the underlying disease process.
How Is Moderate Coronary Artery Calcification Diagnosed?
The diagnosis of coronary artery calcification usually involves imaging tests. One of the most common methods is a coronary calcium scan, also known as a CT coronary angiogram. This test uses a CT scanner to measure the amount of calcium in the coronary arteries. The result is typically given as a calcium score.
Calcium Score: The calcium score is a numerical representation of the amount of calcium detected in the coronary arteries.
A moderate score typically ranges from 100 to 400. This indicates that there is a moderate level of calcification, which is concerning but not necessarily indicative of imminent danger. The higher the score, the more severe the calcification, and the greater the risk of heart disease.
Moderate CAC is also often detected during routine X-rays or chest CT scans. However, the coronary calcium scan remains the gold standard for detecting and quantifying the condition.
What Are the Risks of Moderate Coronary Artery Calcification?
The seriousness of moderate coronary artery calcification lies in its potential to contribute to further cardiovascular complications. While moderate calcification itself may not immediately result in a heart attack, it is a clear sign of ongoing atherosclerosis.
1. Increased Risk of Heart Attack (Myocardial Infarction)
A moderate amount of calcium buildup can lead to the narrowing and hardening of the arteries. This constriction reduces blood flow to the heart muscle, increasing the risk of ischemia (lack of oxygen) and angina (chest pain). If the plaque ruptures or the calcified area destabilizes, it may trigger the formation of a blood clot. This clot can block a coronary artery completely, leading to a heart attack.
2. Stroke Risk
Since the coronary arteries are part of the systemic vascular system, significant coronary calcification may also suggest widespread atherosclerosis, increasing the risk of stroke. If similar plaque buildup occurs in the carotid arteries (the arteries that supply blood to the brain), it can lead to a blockage that causes a stroke.
3. Heart Failure
If the coronary arteries become severely narrowed or blocked due to calcification and atherosclerosis, the heart muscle may not receive enough oxygen-rich blood. This can weaken the heart muscle, leading to heart failure, a condition in which the heart cannot pump blood efficiently.
4. Peripheral Artery Disease
The presence of moderate coronary artery calcification may also be an early indicator of other forms of peripheral artery disease (PAD), where plaque builds up in arteries that supply blood to the limbs. PAD can cause pain, numbness, and a higher risk of infection or gangrene.
What Are the Treatment Options for Moderate Coronary Artery Calcification?
The management of moderate coronary artery calcification focuses on slowing or halting the progression of atherosclerosis, reducing cardiovascular risk, and managing symptoms.
1. Lifestyle Changes
Adopting a healthy lifestyle is the cornerstone of managing coronary artery calcification. Recommendations include:
Diet: Eating a heart-healthy diet low in saturated fats, trans fats, and cholesterol is essential. Incorporating fruits, vegetables, whole grains, and lean proteins can help manage blood pressure and cholesterol levels.
Exercise: Regular physical activity helps strengthen the heart and improve circulation, reducing the risk of further plaque buildup.
Weight Management: Maintaining a healthy weight reduces strain on the heart and can lower blood pressure and cholesterol levels.
Smoking Cessation: Quitting smoking is one of the most important steps in preventing the progression of coronary artery disease.
2. Medications
Several medications can help manage moderate coronary artery calcification:
Statins: These cholesterol-lowering drugs can reduce the progression of atherosclerosis and prevent plaque buildup.
Aspirin: Low-dose aspirin may be prescribed to reduce the risk of blood clot formation in the arteries.
Blood Pressure Medications: Medications like ACE inhibitors, beta-blockers, or angiotensin II receptor blockers (ARBs) help control high blood pressure, a significant contributor to heart disease.
Diabetes Management: If diabetes is present, tight glucose control can help reduce the risk of further plaque buildup.
3. Coronary Intervention
In some cases, when moderate coronary artery calcification leads to significant narrowing of the arteries and symptoms such as chest pain or difficulty breathing, more aggressive treatment may be needed. This can include:
Angioplasty: A procedure where a balloon is used to open up the narrowed artery, and a stent may be placed to keep the artery open.
Coronary Artery Bypass Surgery: If multiple coronary arteries are severely blocked, bypass surgery may be necessary to reroute blood flow to the heart.
Can Moderate Coronary Artery Calcification Be Prevented?
While moderate coronary artery calcification cannot be fully reversed, it can be prevented or its progression slowed through lifestyle changes and medical management. Prevention strategies include:
Regular check-ups with a healthcare provider to monitor cardiovascular risk factors such as cholesterol, blood pressure, and blood sugar.
Early screening for individuals at high risk of heart disease, including those with a family history of CAD or those with other risk factors like smoking, obesity, or diabetes.
Adopting a proactive approach to managing heart health, such as starting medications or therapies as soon as risk factors are identified.
Conclusion
Moderate coronary artery calcification is a significant warning sign of underlying cardiovascular risk. While it does not necessarily indicate an imminent heart attack, it signals the presence of atherosclerosis, which can lead to serious health issues like heart attacks, strokes, and heart failure. Early diagnosis, lifestyle modifications, and appropriate medical management are essential for reducing the risks associated with moderate coronary artery calcification and improving overall heart health.
Related topics: