Pulmonary embolism (PE) and myocardial infarction (MI) are two critical cardiovascular conditions. Both can present suddenly and with life-threatening consequences. While they affect different parts of the cardiovascular system, understanding whether pulmonary embolism can cause myocardial infarction is important for accurate diagnosis and treatment. This article explores the relationship between PE and MI, clarifying the mechanisms, clinical presentation, and management strategies involved.
Understanding Pulmonary Embolism
What is Pulmonary Embolism?
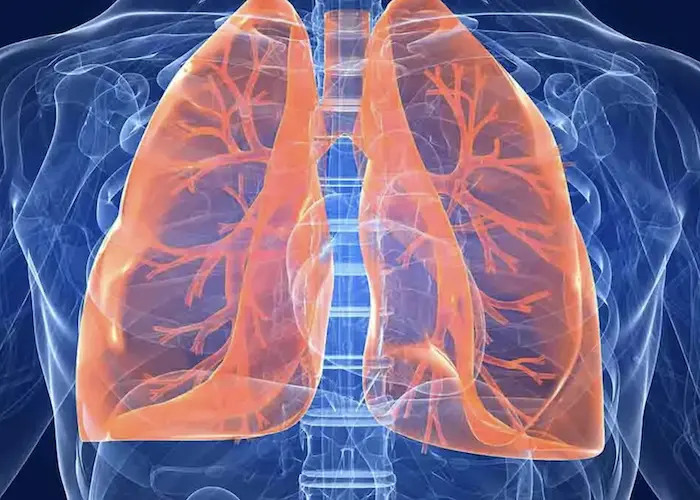
Pulmonary embolism occurs when a blood clot or other material blocks blood flow in the pulmonary arteries, which carry blood from the heart to the lungs. Most often, these clots originate in deep veins of the legs or pelvis, a condition known as deep vein thrombosis (DVT). When the clot travels to the lungs, it obstructs blood flow, causing impaired oxygen exchange and increased pressure on the right side of the heart.
Pathophysiology of Pulmonary Embolism
The obstruction caused by a clot leads to increased pulmonary vascular resistance. This causes strain on the right ventricle (RV), which pumps blood into the lungs. The RV can dilate and fail if the pressure is severe or sudden. Additionally, reduced oxygenation of blood affects the entire body, potentially leading to hypoxia and systemic effects.
Understanding Myocardial Infarction
What is Myocardial Infarction?
Myocardial infarction, commonly called a heart attack, happens when blood flow to a part of the heart muscle (myocardium) is blocked. The blockage usually results from a clot forming over a ruptured atherosclerotic plaque in the coronary arteries. Without oxygen, the heart muscle begins to die, leading to permanent damage if not promptly treated.
Types of Myocardial Infarction
There are several types of MI, classified based on cause and clinical features:
Type 1 MI: Caused by primary coronary artery event like plaque rupture and thrombosis.
Type 2 MI: Caused by imbalance between oxygen supply and demand without coronary thrombosis. This can occur during severe anemia, hypotension, or other stresses.
Other types: Include MI related to coronary artery dissection, spasm, or embolism.
Can Pulmonary Embolism Cause Myocardial Infarction?
Direct vs. Indirect Relationship
Pulmonary embolism and myocardial infarction affect different vascular territories—PE in the pulmonary arteries and MI in the coronary arteries. However, PE can indirectly cause myocardial ischemia and infarction through several mechanisms. Direct causation of MI by PE is rare but possible in specific contexts.
Mechanisms by Which PE May Cause MI
1. Right Ventricular Strain and Ischemia: Acute PE increases pulmonary artery pressure, causing right ventricular overload. The increased workload elevates oxygen demand in the RV. When this demand exceeds supply, ischemia of the RV myocardium may develop, sometimes mimicking an MI.
2. Decreased Left Ventricular Filling: Due to RV failure, less blood returns to the left heart, lowering cardiac output and systemic blood pressure. This can reduce coronary perfusion pressure, potentially triggering ischemia in the left ventricle, especially in patients with pre-existing coronary artery disease.
3. Paradoxical Embolism: In patients with intracardiac shunts such as a patent foramen ovale (PFO), a thrombus from the venous system may bypass the lungs and enter systemic circulation. This can cause coronary artery embolism leading to MI.
4. Hypoxia and Systemic Stress: Severe hypoxia from PE can increase myocardial oxygen demand and reduce supply, leading to myocardial injury or infarction, particularly in vulnerable patients.
Rare Direct Coronary Embolism
In rare cases, a thrombus can embolize directly into the coronary arteries, causing coronary artery occlusion and MI. This is more likely when a right-to-left shunt exists or in the presence of atrial fibrillation or other sources of emboli. Such embolic myocardial infarctions are uncommon but documented.
Clinical Presentation and Diagnosis
Symptoms Overlap and Diagnostic Challenges
Symptoms of PE and MI often overlap: chest pain, shortness of breath, sweating, and palpitations. This overlap can complicate diagnosis, especially in emergency settings. Distinguishing between the two is critical as treatment strategies differ significantly.
Diagnostic Tools
Electrocardiogram (ECG): PE can cause changes mimicking MI, such as ST elevation or T wave inversions. Classic findings in PE include right heart strain patterns (S1Q3T3), but these are not always present.
Cardiac Biomarkers: Troponin elevation can occur in both MI and PE due to myocardial injury. However, the pattern and degree of elevation may differ.
Imaging: CT pulmonary angiography is the gold standard for PE diagnosis. Coronary angiography confirms coronary artery occlusion in MI.
Echocardiography: Useful for assessing right ventricular function and detecting intracardiac shunts, which may indicate paradoxical embolism risk.
Treatment Considerations
Managing Pulmonary Embolism
Treatment of PE primarily involves anticoagulation to prevent clot growth and new clot formation. In massive PE with hemodynamic instability, thrombolysis or surgical embolectomy may be needed. Supportive care includes oxygen therapy and hemodynamic stabilization.
Treating Myocardial Infarction
MI treatment focuses on restoring coronary blood flow through reperfusion strategies like percutaneous coronary intervention (PCI) or thrombolysis. Medications include antiplatelets, anticoagulants, beta-blockers, and statins.
Combined Scenarios and Special Management
When PE and MI coexist or when PE triggers myocardial ischemia, management becomes complex. Anticoagulation for PE must be balanced with antiplatelet therapy for MI. Close monitoring in an intensive care setting is often required. In paradoxical embolism causing MI, closure of cardiac shunts may be considered to prevent recurrence.
Conclusion
While pulmonary embolism primarily affects the lungs and right heart, it can indirectly cause myocardial infarction by increasing right ventricular strain, reducing coronary perfusion, causing hypoxia, or via paradoxical embolism through intracardiac shunts. Direct coronary embolism is rare but possible. Due to overlapping symptoms, careful diagnostic evaluation is essential to differentiate PE from MI or identify when both coexist. Treatment must be tailored to address both conditions when present, balancing anticoagulation and antiplatelet therapies. Understanding this complex relationship enhances clinical care and patient prognosis.
Related topics: