Cardiac arrhythmias are common issues seen in clinical cardiology, with atrial tachycardia (AT) and atrioventricular nodal reentrant tachycardia (AVNRT) being two such arrhythmias that are often confused due to their similarities in symptoms and electrocardiographic (ECG) presentation. However, these two arrhythmias have distinct mechanisms, and proper differentiation is crucial for appropriate management and treatment.
Atrial tachycardia is a type of arrhythmia originating from the atria, while AVNRT is a specific type of supraventricular tachycardia (SVT) resulting from a reentrant circuit within the atrioventricular (AV) node. Understanding the differences between these arrhythmias can help guide both diagnostic approaches and therapeutic strategies.
What Is Atrial Tachycardia?
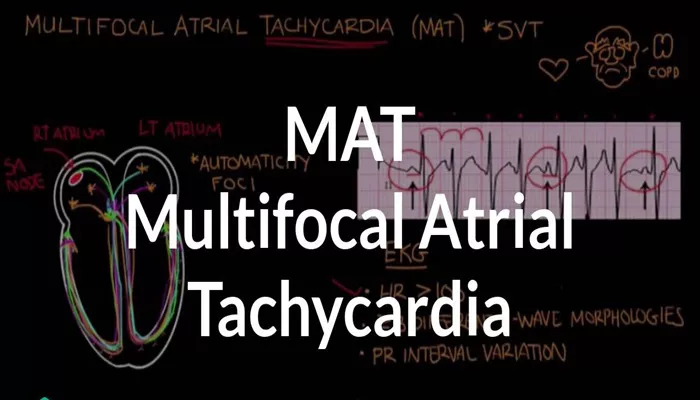
Atrial tachycardia (AT) is a rapid heart rhythm originating from an ectopic focus within the atria. This ectopic focus can arise from anywhere within the atrial tissue, including the pulmonary veins or the right atrium. AT typically has a regular rhythm and can be classified based on its origin, either focal or multifocal.
Mechanism of Atrial Tachycardia
In AT, the rapid heart rate results from a single ectopic focus or multiple ectopic foci firing in the atrium. The heart rate usually ranges between 100 to 250 beats per minute (bpm). The ectopic electrical impulses override the normal sinoatrial (SA) node, causing the atria to contract rapidly and irregularly.
Symptoms of Atrial Tachycardia
Symptoms of atrial tachycardia include palpitations, dizziness, shortness of breath, and occasionally syncope. In some cases, patients may be asymptomatic, especially if the episodes are short and self-limiting.
What is AVNRT?
Atrioventricular nodal reentrant tachycardia (AVNRT) is a type of arrhythmia where the electrical signal travels in a reentrant loop within the AV node. This results in rapid ventricular and atrial contractions due to the abnormal conduction pathway. AVNRT typically occurs in individuals with dual AV nodal pathways, where there is a fast and a slow pathway.
Mechanism of AVNRT
In AVNRT, the electrical impulse enters the AV node, where it can travel along two different pathways—the slow and fast pathways. When an impulse travels down one pathway and is blocked on the way back, the impulse can loop back through the other pathway, creating a reentrant circuit. This causes rapid, regular heartbeats that can range from 150 to 250 bpm.
Symptoms of AVNRT
Symptoms of AVNRT are similar to those of AT and include palpitations, dizziness, and shortness of breath. AVNRT episodes tend to be sudden in onset and termination, with many patients experiencing paroxysms of rapid heart rates.
Key Differences Between Atrial Tachycardia And AVNRT
While atrial tachycardia and AVNRT may present with similar symptoms, there are several distinguishing features that can help differentiate them.
1. ECG Findings: The Key to Diagnosis
Atrial Tachycardia ECG Features:
P-wave morphology: The P-wave in atrial tachycardia is typically abnormal and may have a different shape than normal sinus P-waves.
This reflects the ectopic origin of the impulse.
P-wave timing: The P-wave often precedes the QRS complex by a variable interval. In some cases, the P-wave may be buried in the QRS complex if the tachycardia is occurring at a very high rate.
QRS complex: The QRS complex is usually narrow (unless there is an underlying bundle branch block or ventricular conduction delay).
AVNRT ECG Features:
P-wave morphology: The P-wave in AVNRT may be absent or hidden within the QRS complex, making it difficult to detect on a 12-lead ECG. When visible, the P-wave is often inverted, especially in leads II, III, and aVF.
P-wave timing: The P-wave in AVNRT often follows the QRS complex, typically with a short RP interval.
QRS complex: Like AT, the QRS complex is typically narrow unless there is an accessory pathway or bundle branch block.
2. Heart Rate and Rhythm Regularity
Atrial Tachycardia:
The heart rate in AT is usually slightly faster than in AVNRT, typically between 100 and 250 bpm.
The rhythm is regular, but may vary slightly if multiple ectopic foci are involved.
AVNRT:
AVNRT tends to produce a faster heart rate, usually between 150 and 250 bpm.
The rhythm in AVNRT is typically regular and sustained throughout the episode.
3. Mechanisms of Origin
Atrial Tachycardia:
The origin of AT is always an ectopic focus within the atria. This can be from the right atrium, left atrium, or pulmonary veins.
The focus is typically a single ectopic pacemaker, although in some cases, there may be multiple foci.
AVNRT:
AVNRT occurs due to the reentry circuit within the AV node, typically due to the presence of dual AV nodal pathways (fast and slow).
AVNRT is typically caused by a single reentrant pathway within the AV node.
4. Response to Maneuvers and Medications
Atrial Tachycardia:
Vagal maneuvers, such as the Valsalva maneuver, may not terminate AT. However, adenosine may be helpful in certain cases by slowing down the AV node and revealing the underlying atrial rhythm.
Beta-blockers or calcium channel blockers can be used to control the rate, but AT may require antiarrhythmic medications or catheter ablation for definitive treatment.
AVNRT:
AVNRT is often terminated by vagal maneuvers like the Valsalva maneuver, which increases parasympathetic tone and slows conduction through the AV node.
Adenosine is the drug of choice for terminating AVNRT by blocking the reentry circuit in the AV node.
If maneuvers or medications fail, catheter ablation of the slow pathway within the AV node may be considered.
5. Duration and Onset of Episodes
Atrial Tachycardia:
AT episodes may last longer, ranging from several minutes to hours. The onset is typically gradual.
Episodes of AT can be persistent and may require cardioversion or ablation if they become symptomatic or resistant to pharmacological therapy.
AVNRT:
AVNRT episodes are usually of sudden onset and abrupt termination, often lasting seconds to minutes.
The episodes tend to stop spontaneously, but if they persist, intervention is necessary.
Diagnostic Workup And Evaluation
Differentiating between AT and AVNRT begins with a careful patient history and ECG analysis. For patients with paroxysmal supraventricular tachycardia (PSVT), 12-lead ECG during an episode of arrhythmia is the most crucial diagnostic tool. In some cases, an electrophysiological study (EPS) may be necessary to identify the exact mechanism and origin of the arrhythmia, particularly when the ECG findings are ambiguous.
Electrophysiology Study (EPS) And Ablation
In cases where clinical management does not yield adequate results or the diagnosis is unclear, an electrophysiology study can help map the exact location of the arrhythmia’s origin. During an EPS, catheter ablation may be performed to target the ectopic focus in atrial tachycardia or the slow pathway in AVNRT.
Treatment Strategies
Treatment of Atrial Tachycardia:
Acute management: Rate control with beta-blockers or calcium channel blockers.
Chronic management: Antiarrhythmic drugs like amiodarone or flecainide may be considered. In cases of recurrent or symptomatic AT, catheter ablation may be the most effective treatment.
Treatment of AVNRT:
Acute management: Vagal maneuvers, adenosine, or calcium channel blockers to slow the heart rate.
Chronic management: Long-term management includes medications, such as beta-blockers or calcium channel blockers.
Catheter ablation is often curative in AVNRT, as it targets the reentrant circuit within the AV node.
Conclusion
Differentiating atrial tachycardia from AVNRT is crucial in the management of arrhythmias. By carefully analyzing ECG patterns, considering the patient’s symptoms, and understanding the underlying mechanisms, clinicians can accurately identify the arrhythmia and choose the appropriate treatment. Whether using medications, maneuvers, or catheter ablation, effective management of these arrhythmias improves patient outcomes and quality of life.
Related topics: