Atherosclerosis is a condition that slowly builds over time, affecting the arteries and leading to various cardiovascular diseases, including coronary artery disease (CAD). This article will explore how atherosclerosis leads to CAD by breaking down the process, risk factors, symptoms, and potential outcomes of this debilitating condition. Understanding how atherosclerosis works is essential for preventing and managing coronary artery disease, a leading cause of death worldwide.
Introduction to Atherosclerosis and Coronary Artery Disease
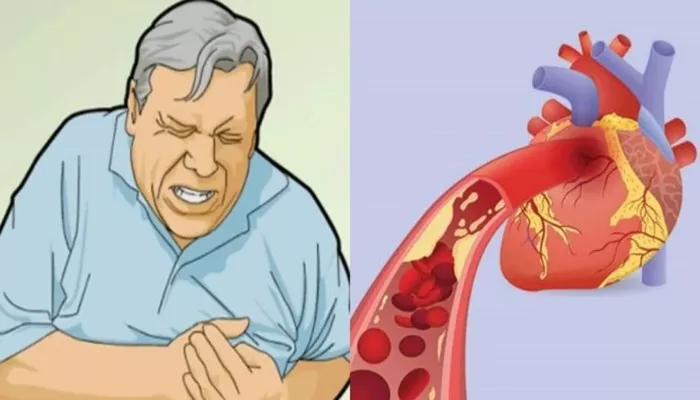
Coronary artery disease (CAD) is one of the most common and serious types of heart disease. It occurs when the coronary arteries—the blood vessels that supply oxygen-rich blood to the heart muscle—become narrowed or blocked due to the buildup of plaque. The condition is most often caused by atherosclerosis, a gradual process in which fatty substances, cholesterol, cellular waste products, and calcium accumulate on the artery walls, forming plaques. These plaques disrupt normal blood flow and may lead to serious complications, including heart attacks.
Atherosclerosis affects many arteries in the body, but when it targets the coronary arteries, it can result in reduced oxygen and nutrients being delivered to the heart muscle, which can damage the heart. Understanding how this process develops is crucial for recognizing the risk factors and preventing CAD.
The Development of Atherosclerosis
Atherosclerosis starts as early as childhood and progresses gradually over time. In the early stages, the artery walls become damaged due to various factors such as high blood pressure, smoking, high cholesterol, and diabetes. When these factors damage the inner lining of the arteries, they allow cholesterol and other substances to accumulate and form plaques.
1. Endothelial Injury
The first step in atherosclerosis involves injury to the endothelium, the thin layer of cells that lines the interior surface of blood vessels. This damage can be caused by various risk factors such as:
High cholesterol: Excess cholesterol in the blood can accumulate on the arterial walls.
High blood pressure: This increases the force on the arterial walls, making them more susceptible to damage.
Smoking: Smoking damages blood vessels and accelerates the development of atherosclerosis.
Diabetes: High blood sugar levels can also contribute to the formation of plaques.
Once the endothelium is damaged, it allows low-density lipoprotein (LDL), often referred to as “bad cholesterol,” to penetrate the arterial walls.
2. Fatty Streak Formation
LDL cholesterol begins to accumulate in the inner layers of the artery walls. The immune system recognizes this cholesterol as a foreign substance and sends white blood cells called macrophages to digest it. However, in the process of trying to clear the cholesterol, macrophages become overwhelmed and transform into foam cells, which then accumulate at the site.
These foam cells eventually form a fatty streak on the arterial walls, which is the earliest visible sign of atherosclerosis. As the fatty streaks build up, they create a thicker plaque, further narrowing the arteries.
3. Plaque Growth and Fibrous Cap Formation
Over time, the fatty streaks evolve into larger plaques composed of a mixture of cholesterol, foam cells, and fibrous tissue.
These plaques are covered by a fibrous cap, which is made up of smooth muscle cells, collagen, and other proteins. The fibrous cap serves as a protective barrier, but if it becomes thin or weak, it can rupture.
The rupturing of a plaque is one of the most dangerous aspects of atherosclerosis. When this happens, the underlying contents, including fatty material and inflammatory cells, are exposed to the bloodstream, triggering the formation of a blood clot. This clot can further obstruct the artery, leading to a complete blockage of blood flow to the heart muscle.
How Atherosclerosis Leads to Coronary Artery Disease
1. Reduced Blood Flow
As the plaques in the coronary arteries grow, they narrow the space available for blood to flow. The heart muscle relies on a constant supply of oxygen-rich blood, and when the arteries are narrowed, this supply is reduced. This condition, known as ischemia, can lead to chest pain or angina, which is one of the early warning signs of CAD.
When the blood flow becomes severely restricted, parts of the heart muscle may begin to die. This can result in a heart attack, also known as a myocardial infarction (MI), where a section of the heart muscle is permanently damaged due to a lack of oxygen.
2. Formation of Blood Clots
As mentioned earlier, the rupture of the fibrous cap that covers a plaque can lead to the formation of blood clots. These clots are dangerous because they can completely block the flow of blood to the heart muscle. When a clot obstructs the coronary artery, it can cause a heart attack.
Even a small clot can have serious consequences. The heart muscle can become deprived of oxygen, leading to cell death.
Depending on the extent of the blockage, this can cause long-term damage to the heart, impairing its ability to pump blood effectively.
3. Complications of CAD
The narrowing and blockage of the coronary arteries due to atherosclerosis can lead to several complications, including:
Heart Attack (Myocardial Infarction): As mentioned earlier, this occurs when a blood clot blocks a coronary artery, causing a portion of the heart muscle to die.
Heart Failure: Prolonged damage to the heart muscle due to repeated ischemia and infarctions can result in heart failure, where the heart is no longer able to pump blood efficiently.
Arrhythmias: The damage to the heart muscle from atherosclerosis can cause abnormal heart rhythms or arrhythmias, which can lead to sudden cardiac arrest if left untreated.
Angina: Chest pain or discomfort that occurs when the heart muscle does not receive enough oxygen-rich blood due to narrowed coronary arteries.
Risk Factors for Atherosclerosis and Coronary Artery Disease
Several factors increase the likelihood of developing atherosclerosis and, subsequently, coronary artery disease. These include:
High cholesterol levels: Elevated LDL cholesterol contributes to plaque buildup in the arteries.
High blood pressure: Damages the arterial walls, accelerating the process of atherosclerosis.
Diabetes: Increases the risk of developing atherosclerosis by promoting inflammation and plaque formation.
Smoking: Damages the blood vessels and increases the likelihood of plaque buildup.
Sedentary lifestyle: Physical inactivity contributes to obesity and other risk factors like high cholesterol and blood pressure.
Unhealthy diet: Diets high in saturated fats and processed foods can raise cholesterol levels and promote plaque formation.
Family history: A family history of heart disease or high cholesterol increases the risk of developing CAD.
Age and gender: Men over 45 and women over 55 are at a higher risk for CAD, and the risk increases with age.
Symptoms of Coronary Artery Disease
In the early stages of atherosclerosis, individuals may not experience any noticeable symptoms. However, as the condition progresses, symptoms of coronary artery disease may develop, including:
Chest pain (Angina): A feeling of pressure, heaviness, or tightness in the chest.
Shortness of breath: Difficulty breathing, especially with exertion.
Fatigue: Feeling unusually tired or fatigued even after minimal physical activity.
Palpitations: An irregular or rapid heartbeat.
Heart attack symptoms: Pain or discomfort in the chest, arms, back, neck, or jaw; dizziness; nausea; and sweating.
If any of these symptoms occur, immediate medical attention is necessary.
Preventing Atherosclerosis and Coronary Artery Disease
Preventing atherosclerosis and CAD requires addressing the risk factors associated with the condition. Some important lifestyle changes include:
Healthy diet: Focus on a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
Regular physical activity: Exercise helps lower cholesterol, reduce blood pressure, and improve heart health.
Avoid smoking: Smoking cessation is one of the most important steps in preventing CAD.
Manage diabetes and high blood pressure: Proper management of diabetes and blood pressure can prevent the development of atherosclerosis.
Medications: In some cases, medications such as statins may be prescribed to help manage cholesterol levels.
Conclusion
Atherosclerosis plays a significant role in the development of coronary artery disease. The buildup of plaque in the coronary arteries gradually narrows these blood vessels, restricting blood flow to the heart muscle. This can lead to chest pain, heart attacks, and other serious complications. Understanding the processes behind atherosclerosis and its impact on the cardiovascular system is essential for prevention and effective treatment of coronary artery disease.
Related topics: