Supraventricular tachycardia (SVT) is a term that encompasses a variety of rapid heart rhythms originating above the ventricles, typically in the atria or the atrioventricular (AV) node. SVT can lead to symptoms such as palpitations, dizziness, shortness of breath, and, in some cases, chest pain. Treatment for SVT often involves medications, lifestyle changes, and sometimes procedures like catheter ablation. This article will explore the medications used to treat SVT, their mechanisms of action, indications, and potential side effects, while also discussing other management strategies.
Understanding Supraventricular Tachycardia (SVT)
What is SVT
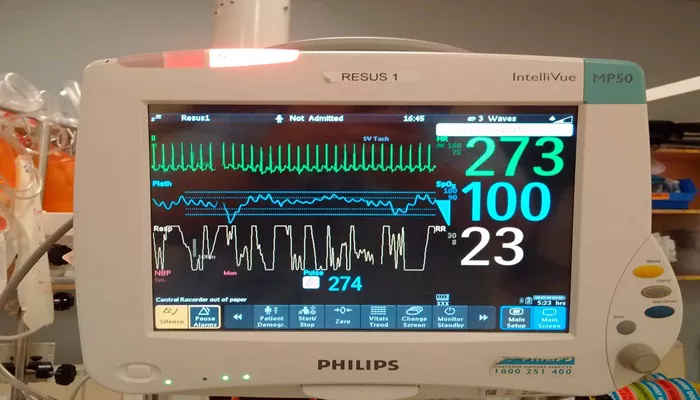
SVT is characterized by an abnormally fast heart rate that originates from the atria or the AV junction. The heart rate in SVT can exceed 100 beats per minute and may reach rates of 200 to 300 beats per minute. The condition can be classified into several types, including.
Atrial Fibrillation (AFib): An irregular and often rapid heart rhythm.
Atrial Flutter: A rapid but regular heart rhythm originating in the atria.
AV Nodal Reentrant Tachycardia (AVRT): A reentrant circuit involving the AV node.
Atrial Tachycardia: Rapid heartbeats originating from the atrial tissue.
Symptoms of SVT
Symptoms of SVT can vary based on the individual and the duration of the episode. Common symptoms include.
Palpitations or a racing heart
Dizziness or lightheadedness
Shortness of breath
Chest discomfort or pain
Fatigue
In some cases, individuals may experience no symptoms at all, especially if the episodes are brief.
Causes of SVT
SVT can be triggered by various factors, including:
Structural Heart Disease: Conditions such as cardiomyopathy or congenital heart defects.
Electrolyte Imbalances: Abnormal levels of potassium, magnesium, or calcium can affect heart rhythm.
Stimulants: Caffeine, nicotine, alcohol, and certain medications can provoke SVT.
Stress and Anxiety: Emotional stress can lead to episodes of SVT.
Hyperthyroidism: An overactive thyroid can increase heart rate and trigger SVT.
Medications Used to Treat SVT
The treatment of SVT often involves the use of medications to control heart rate, restore normal rhythm, and prevent future episodes. The choice of medication depends on the specific type of SVT, the frequency and severity of episodes, and the presence of underlying health conditions.
Beta-Blockers
Beta-blockers are a class of medications that block the effects of adrenaline on the heart. They are commonly used to manage various cardiovascular conditions, including SVT.
Mechanism of Action
Beta-blockers work by blocking beta-adrenergic receptors, leading to a decrease in heart rate and contractility. This results in reduced myocardial oxygen demand and can help control episodes of SVT.
Commonly Used Beta-Blockers
Metoprolol (Lopressor, Toprol XL): Often used for its cardioselective properties, metoprolol is effective in managing SVT and reducing heart rate.
Atenolol (Tenormin): Another cardioselective beta-blocker, atenolol is commonly prescribed for hypertension and arrhythmias.
Propranolol (Inderal): A non-selective beta-blocker that can be effective in controlling SVT, particularly in patients with anxiety-related episodes.
Indications
Beta-blockers are indicated for patients with recurrent SVT, especially if they have concomitant conditions such as hypertension or anxiety.
Side Effects
Common side effects of beta-blockers include fatigue, dizziness, bradycardia (slow heart rate), and potential worsening of asthma or chronic obstructive pulmonary disease (COPD) due to bronchoconstriction.
Calcium Channel Blockers
Calcium channel blockers are another class of medications used to treat SVT. They work by inhibiting calcium entry into cardiac and smooth muscle cells, leading to decreased heart rate and contractility.
Mechanism of Action
Calcium channel blockers primarily affect the AV node, slowing conduction and helping to terminate episodes of SVT.
Commonly Used Calcium Channel Blockers
Diltiazem (Cardizem): Often used for rate control in patients with SVT and atrial fibrillation.
Verapamil (Calan, Isoptin): Effective in managing SVT by slowing conduction through the AV node.
Indications
Calcium channel blockers are indicated for patients with SVT who may not tolerate beta-blockers or in cases where rapid control of heart rate is needed.
Side Effects
Potential side effects of calcium channel blockers include hypotension (low blood pressure), dizziness, bradycardia, and constipation, particularly with verapamil.
Adenosine
Adenosine is a unique medication used primarily for the acute treatment of SVT. It acts rapidly to restore normal sinus rhythm.
Mechanism of Action
Adenosine works by temporarily blocking conduction through the AV node, which can interrupt reentrant circuits responsible for SVT. It is administered as a rapid intravenous bolus.
Indications
Adenosine is indicated for the acute termination of paroxysmal SVT, especially in emergency settings.
Side Effects
Common side effects of adenosine include flushing, chest discomfort, shortness of breath, and a transient feeling of impending doom. These effects are usually brief and resolve quickly.
Antiarrhythmic Medications
Antiarrhythmic medications are used to restore and maintain normal heart rhythm in patients with SVT.
Mechanism of Action
Antiarrhythmics work through various mechanisms, including sodium channel blockade, potassium channel blockade, and calcium channel blockade, depending on the specific drug class.
Commonly Used Antiarrhythmics
Flecainide (Tambocor): A class IC antiarrhythmic used for atrial fibrillation and SVT.
Propafenone (Rythmol): Another class IC antiarrhythmic effective for controlling SVT.
Sotalol (Betapace): A class III antiarrhythmic that can be used for rhythm control in SVT.
Indications
Antiarrhythmic medications are indicated for patients with recurrent SVT who do not respond to beta-blockers or calcium channel blockers or for those who have frequent symptomatic episodes.
Side Effects
Potential side effects of antiarrhythmic medications can include dizziness, fatigue, proarrhythmia (the potential to cause new or worsening arrhythmias), and other systemic effects depending on the specific drug.
Digoxin
Digoxin is a cardiac glycoside that can be used in certain cases of SVT, particularly in patients with heart failure or those who have not responded to other treatments.
Mechanism of Action
Digoxin works by increasing vagal tone and slowing conduction through the AV node, which can help control heart rate during episodes of SVT.
Indications
Digoxin is indicated for patients with SVT who have underlying heart failure or reduced ejection fraction.
Side Effects
Common side effects of digoxin include nausea, vomiting, dizziness, and visual disturbances (such as yellow-green halos). Digoxin toxicity can occur, especially in patients with renal impairment or electrolyte imbalances.
Non-Pharmacological Management of SVT
In addition to medications, various non-pharmacological strategies can be employed to manage SVT.
Vagal Maneuvers
Vagal maneuvers are physical techniques that stimulate the vagus nerve, which can help slow the heart rate and terminate episodes of SVT. Common maneuvers include.
Valsalva Maneuver: Involves forcefully exhaling against a closed airway.
Carotid Sinus Massage: Gently massaging the carotid artery in the neck can stimulate the vagus nerve and slow heart rate.
Diving Reflex: Immersing the face in cold water can activate the vagal response.
Catheter Ablation
Catheter ablation is a minimally invasive procedure used to treat recurrent SVT. It involves threading a catheter through the blood vessels to the heart to identify and destroy the abnormal electrical pathways responsible for SVT.
Indications
Catheter ablation is indicated for patients with recurrent symptomatic SVT who do not respond to medical therapy or prefer a definitive treatment option.
Success Rates
The success rates for catheter ablation vary depending on the type of SVT but can be as high as 90% for certain types, such as AV nodal reentrant tachycardia.
Lifestyle Modifications
Patients with SVT can benefit from lifestyle modifications to reduce the frequency of episodes. Recommendations may include.
Avoiding Stimulants: Reducing or eliminating caffeine, nicotine, and alcohol can help manage SVT.
Stress Management: Practicing relaxation techniques such as yoga, meditation, or deep breathing exercises can help reduce stress-related SVT episodes.
Regular Exercise: Engaging in regular physical activity can improve cardiovascular health and reduce the risk of arrhythmias.
Conclusion
Supraventricular tachycardia (SVT) is a common arrhythmia that can significantly impact a patient’s quality of life. The management of SVT often involves a combination of medications, lifestyle changes, and non-pharmacological interventions.
Medications such as beta-blockers, calcium channel blockers, adenosine, antiarrhythmics, and digoxin play a crucial role in controlling heart rate and preventing recurrent episodes. Understanding the mechanisms, indications, and potential side effects of these medications is essential for effective management.
Related Topics: