Bradycardia is a condition defined by a heart rate slower than 60 beats per minute. It can cause symptoms like dizziness, fatigue, and fainting, or it may be asymptomatic. Bradycardia results from many causes, including sinus node dysfunction, heart block, or drug effects. One important medication used in acute management of symptomatic bradycardia is atropine. This article focuses on the initial dose of atropine for bradycardia and provides detailed clinical insights into its administration, pharmacology, and safety.
Understanding Bradycardia
Bradycardia can be physiological or pathological. Athletes may have normal low heart rates, while others experience bradycardia due to disease. When heart rate is too low, cardiac output drops, leading to poor tissue perfusion and symptoms. Causes include:
- Sinus node dysfunction
- Atrioventricular (AV) block
- Medications such as beta-blockers or calcium channel blockers
- Hypothyroidism
- Electrolyte imbalances
Pharmacology of Atropine
Atropine is an anticholinergic agent that blocks the parasympathetic influence on the heart. It competitively inhibits acetylcholine at muscarinic receptors, particularly the M2 receptors in the sinoatrial (SA) and atrioventricular (AV) nodes.
This blockade reduces vagal tone, allowing the heart rate to increase.
Mechanism of Action
Atropine increases the firing rate of the SA node and improves conduction through the AV node. It is effective in bradycardia caused by increased vagal tone or AV nodal block but less effective in infranodal blocks or myocardial damage.
Pharmacokinetics
Atropine is rapidly absorbed when administered intravenously. It has a quick onset of action, usually within 1 to 2 minutes, and its effects last approximately 2 to 4 hours. It crosses the blood-brain barrier, which may cause central nervous system effects in some cases.
Indications for Atropine in Bradycardia
Atropine is indicated for symptomatic bradycardia where low heart rate causes symptoms such as hypotension, altered mental status, chest pain, or signs of shock. It is often used in emergency settings to stabilize the patient.
When to Use Atropine
Use atropine in cases of:
- Sinus bradycardia with symptoms
- First-degree or second-degree AV block with symptoms
- Bradycardia induced by vagal stimulation
When Not to Use Atropine
Atropine is ineffective or contraindicated in:
- Third-degree AV block where the escape rhythm is infranodal
- Bradycardia caused by hypothermia
- Bradycardia due to drug overdose such as beta-blockers or calcium channel blockers (other treatments preferred)
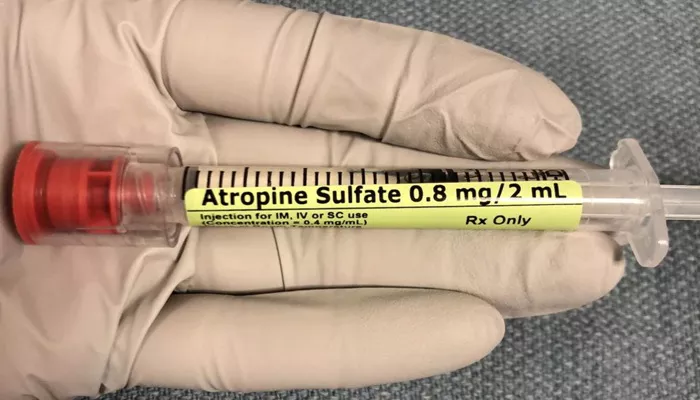
Initial Dose of Atropine for Bradycardia
The initial dose of atropine recommended for symptomatic bradycardia in adults is 0.5 mg intravenously. This dose may be repeated every 3 to 5 minutes as needed.
Dosing Guidelines
- Initial dose: 0.5 mg IV push
- Repeat dose every 3 to 5 minutes if bradycardia persists
- Maximum total dose: 3 mg
Rationale for Dose Selection
The 0.5 mg dose is sufficient to block muscarinic receptors and counteract vagal stimulation. Lower doses (<0.5 mg) can paradoxically cause further slowing of the heart rate, so they are avoided. The upper limit of 3 mg reduces the risk of atropine toxicity.
Administration Considerations
Atropine should be administered rapidly intravenously to ensure fast onset. It can be given via peripheral or central venous access. Continuous monitoring of heart rate and blood pressure is essential during administration.
Monitoring
Monitor for:
- Improvement in heart rate and symptoms
- Adverse effects such as tachycardia, dry mouth, blurred vision, or confusion
- Signs of atropine overdose, which may require supportive care
Adverse Effects
Common side effects include dry mouth, blurred vision, urinary retention, and tachycardia. Central nervous system effects such as agitation or confusion may occur, especially in elderly patients.
Special Populations
Children
The initial dose of atropine for bradycardia in children is typically 0.02 mg/kg intravenously. The minimum dose should not be less than 0.1 mg, and the maximum single dose is 0.5 mg.
Elderly Patients
Older adults may be more sensitive to atropine. Start with the standard initial dose but monitor closely for adverse effects.
Patients with Heart Transplants
Atropine may be less effective in heart transplant recipients because the heart is denervated.
Alternatives and Additional Treatments for Bradycardia
If atropine is ineffective, other interventions include:
Transcutaneous Pacing
This is a temporary measure that uses electrical impulses to stimulate the heart when drugs fail.
Other Medications
Drugs like dopamine or epinephrine infusion may be used to increase heart rate and blood pressure.
Treating Underlying Causes
Address electrolyte imbalances, medication side effects, or ischemia contributing to bradycardia.
Conclusion
Atropine remains a first-line treatment for symptomatic bradycardia. The recommended initial adult dose is 0.5 mg IV, repeated every 3-5 minutes up to a maximum of 3 mg. Prompt administration can reverse vagally mediated bradycardia and improve patient outcomes. Careful monitoring during and after administration is essential to detect efficacy and adverse effects. In cases where atropine fails, pacing and other pharmacologic agents are important alternatives.
Related topics: