Orthostatic hypotension (OH) is a condition characterized by a significant drop in blood pressure when a person stands up from a sitting or lying position. This sudden change can lead to symptoms such as dizziness, lightheadedness, and fainting. For many individuals experiencing orthostatic hypotension, a common question arises: “How many days does orthostatic hypotension last?” Understanding the duration of this condition is essential for effective management and improving quality of life. In this article, we will explore the nature of orthostatic hypotension, its causes, symptoms, potential duration, and management strategies.
Understanding Orthostatic Hypotension
Definition and Mechanism
Orthostatic hypotension occurs when there is a significant drop in blood pressure upon standing, typically defined as a decrease of at least 20 mm Hg in systolic blood pressure or 10 mm Hg in diastolic blood pressure within three minutes of standing. This drop can lead to inadequate blood flow to the brain and other vital organs.
The body normally compensates for the gravitational effects of standing through several mechanisms:
Heart Rate Increase: The heart beats faster to maintain blood flow.
Vasoconstriction: Blood vessels constrict to increase vascular resistance and maintain blood pressure.
Blood Redistribution: Blood is redirected from non-essential areas to critical organs like the brain and heart.
In individuals with orthostatic hypotension, these compensatory mechanisms fail, leading to symptoms.
Symptoms of Orthostatic Hypotension
The symptoms of orthostatic hypotension can vary in severity and may include:
Dizziness or Lightheadedness: Often experienced when standing up quickly.
Fainting (Syncope): A sudden loss of consciousness due to insufficient blood flow to the brain.
Blurred Vision: Changes in blood flow can affect vision temporarily.
Weakness or Fatigue: A general feeling of tiredness may accompany the condition.
Nausea: Some individuals may feel nauseated when standing.
These symptoms can significantly impact daily activities and quality of life, particularly for older adults and those with pre-existing health conditions.
Causes of Orthostatic Hypotension
Understanding the causes of orthostatic hypotension is critical to determining its duration and appropriate management. Common causes include:
Dehydration
Inadequate fluid intake or excessive fluid loss (due to sweating, vomiting, diarrhea, or fever) can lead to reduced blood volume, exacerbating orthostatic hypotension.
Medications
Certain medications can contribute to orthostatic hypotension, including:
Diuretics: These medications can lead to dehydration and reduced blood volume.
Antihypertensives: Medications designed to lower blood pressure may cause excessive drops in blood pressure upon standing.
Antidepressants: Some antidepressants can affect blood pressure regulation.
Neurological Disorders
Conditions such as Parkinson’s disease, multiple system atrophy, and diabetic neuropathy can impair the body’s ability to regulate blood pressure upon standing.
Cardiovascular Conditions
Heart conditions, such as heart failure or arrhythmias, can also contribute to orthostatic hypotension by affecting the heart’s ability to pump blood effectively.
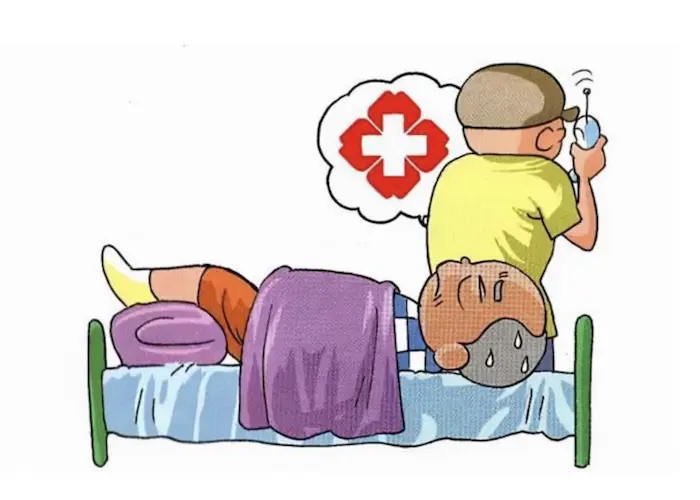
Prolonged Bed Rest
Extended periods of immobility can lead to deconditioning of the cardiovascular system, making it more difficult for the body to adjust to changes in posture.
Age
Older adults are at higher risk for orthostatic hypotension due to age-related changes in blood pressure regulation and cardiovascular health.
Duration of Orthostatic Hypotension
The duration of orthostatic hypotension can vary widely depending on several factors, including its underlying cause, individual health status, and the effectiveness of management strategies. Here, we will explore different scenarios regarding the duration of orthostatic hypotension.
Transient Orthostatic Hypotension
In some cases, orthostatic hypotension may be transient, meaning it occurs temporarily due to specific circumstances such as dehydration, illness, or medication changes. In these instances, symptoms may last for a few hours to several days, depending on the underlying cause.
Example:
Dehydration: If an individual experiences orthostatic hypotension due to dehydration from illness, rehydration can lead to a return to normal blood pressure levels and symptom resolution within a day or two.
Chronic Orthostatic Hypotension
For individuals with chronic orthostatic hypotension, particularly those with underlying health conditions or age-related changes, the condition may persist for weeks, months, or even longer. Chronic cases may require ongoing management to alleviate symptoms.
Example:
Chronic Conditions: Individuals with diabetes may experience chronic orthostatic hypotension due to autonomic neuropathy. While the condition may persist, lifestyle modifications, medication adjustments, and regular monitoring can help manage symptoms effectively.
Medication-Induced Orthostatic Hypotension
If orthostatic hypotension is caused by medications, the duration of symptoms may depend on the half-life of the medication and how quickly the body adjusts to changes in the medication regimen.
Example:
Medication Review: A healthcare provider may adjust the dosage of antihypertensive medications or switch to alternatives that have a lesser impact on blood pressure regulation. In such cases, symptoms may improve within days to weeks after the medication change.
Age-Related Orthostatic Hypotension
In older adults, orthostatic hypotension may be linked to age-related physiological changes. While the condition may not entirely resolve, it can often be managed with lifestyle modifications and medical interventions.
Example:
Age-Related Changes: Older adults may experience orthostatic hypotension due to reduced cardiovascular responsiveness. While this may not completely go away, strategies such as gradual position changes, hydration, and medication adjustments can help manage symptoms.
Lifestyle Modifications
Implementing lifestyle changes can significantly improve symptoms of orthostatic hypotension, and in some cases, lead to resolution.
Strategies Include:
Hydration: Increasing fluid intake to maintain blood volume.
Dietary Changes: Eating smaller, more frequent meals to prevent postprandial hypotension (low blood pressure after meals).
Gradual Position Changes: Encouraging slow transitions from lying or sitting to standing can help prevent symptoms.
Compression Stockings: Wearing compression garments can help reduce blood pooling in the legs.
Physical Therapy and Exercise
Engaging in regular physical activity can improve cardiovascular health and enhance the body’s ability to regulate blood pressure. For some individuals, a structured exercise program may lead to significant improvements in symptoms.
Example:
Exercise Programs: Physical therapy focusing on strength training and balance can help improve overall cardiovascular function and reduce episodes of orthostatic hypotension.
Management of Orthostatic Hypotension
Effective management of orthostatic hypotension is crucial, especially for individuals experiencing chronic symptoms. Here are some strategies that can help:
Hydration
Maintaining adequate hydration is essential for managing orthostatic hypotension. Increasing fluid intake can help increase blood volume and reduce symptoms.
Tips:
Drink Water Regularly: Aim to drink water throughout the day, especially during hot weather or after exercise.
Electrolyte Solutions: Consider electrolyte drinks to help maintain fluid balance.
Dietary Adjustments
Making specific dietary changes can help manage orthostatic hypotension:
Increase Salt Intake: If advised by a healthcare provider, increasing dietary sodium can help retain fluid and improve blood volume.
Eat Smaller Meals: Consuming smaller, more frequent meals can prevent large drops in blood pressure after eating.
Gradual Position Changes
Encouraging slow transitions from lying or sitting to standing can help prevent symptoms of orthostatic hypotension.
Recommendations:
Sit on the Edge of the Bed: Before standing, sit on the edge of the bed for a few minutes to allow the body to adjust.
Use Support: If feeling unsteady, use furniture or a wall for support when standing.
Compression Garments
Wearing compression stockings can help reduce blood pooling in the legs, which is particularly beneficial for individuals with orthostatic hypotension.
Recommendations:
Choose the Right Fit: Ensure that compression stockings fit properly and are worn according to the manufacturer’s instructions.
Medication Management
For some individuals, medication may be necessary to manage orthostatic hypotension:
Fludrocortisone: This medication helps increase blood volume and is often prescribed for orthostatic hypotension.
Midodrine: This medication works by constricting blood vessels and increasing blood pressure.
Monitoring and Follow-Up
Regular follow-up with healthcare providers is essential for managing orthostatic hypotension effectively. This may include:
Routine Blood Pressure Checks: Monitoring blood pressure regularly can help identify trends and adjust treatment as needed.
Assessment of Symptoms: Discussing any changes in symptoms or new concerns with healthcare providers.
Conclusion
Orthostatic hypotension is a condition that can significantly impact an individual’s quality of life. The duration of orthostatic hypotension varies widely depending on several factors, including its underlying cause, individual health status, and the effectiveness of management strategies. While transient cases of orthostatic hypotension may resolve quickly, chronic cases may require ongoing management.
Understanding the nature of orthostatic hypotension, recognizing its symptoms, and implementing effective management strategies can help individuals lead healthier, more active lives while minimizing the risks associated with this condition. By staying informed and working closely with healthcare providers, individuals can effectively manage their symptoms and improve their overall well-being.
Related Topics: