Metabolic diseases are disorders that disrupt the body’s normal metabolic processes, leading to a range of health complications. Among these, three major conditions stand out due to their prevalence and impact on public health: diabetes mellitus, metabolic syndrome, and obesity. Collectively referred to as the “Big Metabolic 3,” these diseases are interrelated and contribute significantly to morbidity and mortality worldwide. This article will delve into each of these conditions, exploring their definitions, causes, symptoms, complications, diagnosis, treatment options, and the importance of prevention.
Understanding Metabolic Diseases
Definition of Metabolic Diseases
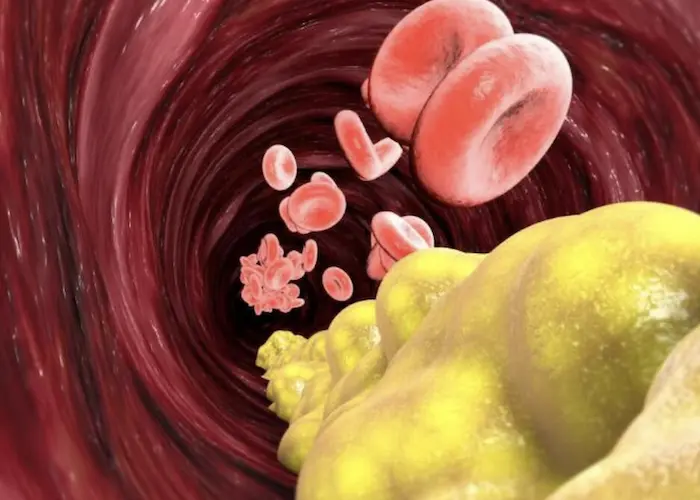
Metabolic diseases encompass a variety of disorders that affect the body’s ability to convert food into energy or utilize nutrients effectively. These diseases can arise from genetic factors, hormonal imbalances, lifestyle choices, or environmental influences. The consequences of metabolic diseases can be severe, leading to complications such as cardiovascular disease, kidney failure, and even death if left untreated.
The Interconnectedness of the Big Metabolic 3
The Big Metabolic 3—diabetes mellitus, metabolic syndrome, and obesity—are closely related. Each condition can influence the others, creating a cycle of health issues that can be challenging to break. For example, obesity is a significant risk factor for developing type 2 diabetes and metabolic syndrome, while these conditions can further exacerbate obesity-related health problems.
Diabetes Mellitus
Diabetes mellitus is a chronic condition characterized by high blood sugar levels (hyperglycemia) due to the body’s inability to produce or effectively use insulin. There are two primary types of diabetes:
Type 1 Diabetes: An autoimmune condition where the immune system attacks insulin-producing beta cells in the pancreas, leading to little or no insulin production. This type typically develops in childhood or adolescence but can occur at any age.
Type 2 Diabetes: The more common form of diabetes, characterized by insulin resistance and relative insulin deficiency. It is often associated with obesity and a sedentary lifestyle and usually develops in adults, although it is increasingly being diagnosed in children and adolescents.
Causes
The causes of diabetes vary depending on the type:
Type 1 Diabetes: The exact cause is unknown, but genetic predisposition and environmental factors (such as viral infections) may play a role.
Type 2 Diabetes: This type is primarily linked to lifestyle factors, including obesity, physical inactivity, poor diet, and genetic predisposition.
Symptoms
Common symptoms of diabetes include:
- Increased thirst and hunger
- Frequent urination
- Fatigue
- Blurred vision
- Slow-healing wounds
- Unexplained weight loss (more common in type 1)
Complications
If left unmanaged, diabetes can lead to severe complications, including:
Cardiovascular Disease: Diabetes significantly increases the risk of heart disease and stroke.
Neuropathy: High blood sugar levels can damage nerves, leading to pain, tingling, or loss of sensation, particularly in the extremities.
Retinopathy: Damage to the blood vessels in the retina can lead to vision loss.
Nephropathy: Diabetes can damage the kidneys, leading to kidney failure.
Foot Complications: Poor circulation and nerve damage can lead to foot ulcers and infections.
Diagnosis
Diabetes is diagnosed through various blood tests, including:
Fasting Plasma Glucose Test: Measures blood sugar levels after fasting for at least eight hours.
Oral Glucose Tolerance Test (OGTT): Measures blood sugar levels before and two hours after consuming a sugary drink.
Hemoglobin A1c Test: Provides an average blood sugar level over the past two to three months.
Treatment
Management of diabetes involves a combination of lifestyle changes and medical interventions:
Lifestyle Modifications: A balanced diet, regular physical activity, and weight management are crucial for controlling blood sugar levels.
Medications: Type 1 diabetes requires insulin therapy, while type 2 diabetes may be managed with oral medications or insulin.
Monitoring: Regular blood sugar monitoring is essential for managing diabetes effectively.
Metabolic Syndrome
Metabolic syndrome is a cluster of conditions that occur together, increasing the risk of heart disease, stroke, and type 2 diabetes. It is characterized by the presence of at least three of the following risk factors:
- Abdominal obesity (waist circumference greater than 40 inches in men and 35 inches in women)
- High blood pressure (≥130/85 mmHg)
- Elevated fasting blood sugar levels (≥100 mg/dL)
- High triglyceride levels (≥150 mg/dL)
- Low high-density lipoprotein (HDL) cholesterol levels (less than 40 mg/dL in men and 50 mg/dL in women)
Causes
The exact cause of metabolic syndrome is multifactorial and includes:
Obesity: Excess fat, particularly visceral fat, contributes to insulin resistance.
Physical Inactivity: Sedentary lifestyles are a significant risk factor.
Genetic Factors: Family history can increase susceptibility.
Hormonal Changes: Hormonal imbalances can influence metabolism and fat distribution.
Symptoms
Metabolic syndrome often has no clear symptoms, but individuals may notice:
- Increased waist circumference
- Fatigue
- High blood pressure readings
- Elevated blood sugar levels
Complications
Complications associated with metabolic syndrome include:
Cardiovascular Disease: Increased risk of heart attack and stroke.
Type 2 Diabetes: Higher likelihood of developing diabetes due to insulin resistance.
Fatty Liver Disease: Accumulation of fat in the liver can lead to liver damage.
Diagnosis
Diagnosis of metabolic syndrome is based on the presence of at least three of the risk factors mentioned above. Healthcare providers typically assess waist circumference, blood pressure, and laboratory values for blood sugar and lipid levels.
Treatment
Management of metabolic syndrome focuses on lifestyle changes and may include:
Weight Loss: Even modest weight loss can significantly reduce risk factors.
Physical Activity: Regular exercise improves insulin sensitivity and cardiovascular health.
Dietary Changes: A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins is recommended.
Medications: Depending on individual risk factors, medications may be prescribed to manage blood pressure, cholesterol, and blood sugar levels.
Obesity
Obesity is defined as an excessive accumulation of body fat that presents a risk to health. It is typically measured using the body mass index (BMI), with a BMI of 30 or higher classified as obese. Obesity is a significant risk factor for developing other metabolic diseases, including diabetes and metabolic syndrome.
Causes
Obesity is a complex condition influenced by multiple factors:
Genetic Factors: Genetics can affect metabolism, fat distribution, and appetite regulation.
Environmental Factors: Access to unhealthy foods, sedentary lifestyles, and socioeconomic status can contribute to obesity.
Behavioral Factors: Poor dietary choices and lack of physical activity are significant contributors.
Hormonal Factors: Hormonal imbalances can influence appetite and metabolism.
Symptoms
Symptoms of obesity may include:
- Excess body fat, particularly around the abdomen
- Shortness of breath during physical activity
- Fatigue
- Joint pain
- Increased sweating
Complications
Obesity is associated with numerous health complications, including:
Type 2 Diabetes: Significant link between obesity and the development of insulin resistance.
Cardiovascular Disease: Increased risk of heart disease, hypertension, and stroke.
Sleep Apnea: Obesity can lead to breathing problems during sleep.
Certain Cancers: Increased risk of various cancers, including breast, colon, and endometrial cancer.
Joint Problems: Increased stress on joints can lead to osteoarthritis.
Diagnosis
Obesity is diagnosed using the BMI calculation:
BMI Calculation: Weight (kg) / Height (m²). A BMI of 30 or higher indicates obesity.
Treatment
Management of obesity typically involves a combination of lifestyle changes, behavioral therapy, and medical interventions:
Lifestyle Modifications: Adopting a healthy diet and increasing physical activity are essential.
Behavioral Therapy: Counseling and support groups can help individuals make lasting lifestyle changes.
Medications: Prescription medications may be used to aid weight loss in certain individuals.
Surgery: Bariatric surgery may be an option for individuals with severe obesity who have not had success with other weight loss methods.
The Relationship Between the Big Metabolic 3
The Big Metabolic 3—diabetes, metabolic syndrome, and obesity—are interrelated and often coexist. Understanding their connections is crucial for effective prevention and management:
Obesity as a Risk Factor: Obesity is a primary risk factor for both type 2 diabetes and metabolic syndrome. Excess body fat, particularly visceral fat, contributes to insulin resistance and other metabolic abnormalities.
Shared Pathophysiology: All three conditions share common underlying mechanisms, including insulin resistance, inflammation, and dyslipidemia (abnormal lipid levels).
Compounding Effects: The presence of one condition can exacerbate the others. For example, individuals with obesity are more likely to develop diabetes, while those with diabetes are at increased risk for cardiovascular complications associated with metabolic syndrome.
Prevention Strategies
Lifestyle Modifications
Preventing the Big Metabolic 3 involves adopting healthy lifestyle habits:
Balanced Diet: Emphasizing whole foods, fruits, vegetables, lean proteins, and healthy fats while minimizing processed foods, sugars, and unhealthy fats.
Regular Physical Activity: Engaging in at least 150 minutes of moderate-intensity aerobic exercise per week, along with strength training.
Weight Management: Maintaining a healthy weight through a combination of diet and exercise.
Regular Health Screenings
Early detection and management of risk factors are crucial for preventing the Big Metabolic 3:
Routine Check-Ups: Regular visits to healthcare providers for monitoring blood pressure, cholesterol levels, and blood sugar.
Screening for Risk Factors: Identifying individuals at risk for obesity, diabetes, and metabolic syndrome through assessments of BMI, waist circumference, and family history.
Education and Support
Providing education and support to individuals and communities can help promote healthy behaviors:
Community Programs: Initiatives that encourage physical activity, healthy eating, and lifestyle changes can have a positive impact on public health.
Patient Education: Healthcare providers should educate patients about the risks associated with obesity, diabetes, and metabolic syndrome, as well as strategies for prevention and management.
Conclusion
The Big Metabolic 3—diabetes mellitus, metabolic syndrome, and obesity—represent significant public health challenges that require a multifaceted approach for prevention and management. Understanding the interconnectedness of these conditions is crucial for healthcare providers, patients, and communities alike.
By adopting healthy lifestyle habits, promoting regular health screenings, and providing education and support, we can work towards reducing the prevalence of these metabolic diseases. Early intervention and comprehensive management strategies can improve health outcomes and enhance the quality of life for individuals affected by these conditions.
As we continue to address the rising rates of obesity, diabetes, and metabolic syndrome globally, it is essential to foster a culture of health and wellness that empowers individuals to take charge of their health and make informed choices. Through collaboration among healthcare professionals, public health initiatives, and community support, we can combat the Big Metabolic 3 and create a healthier future for all.
Related Topics: