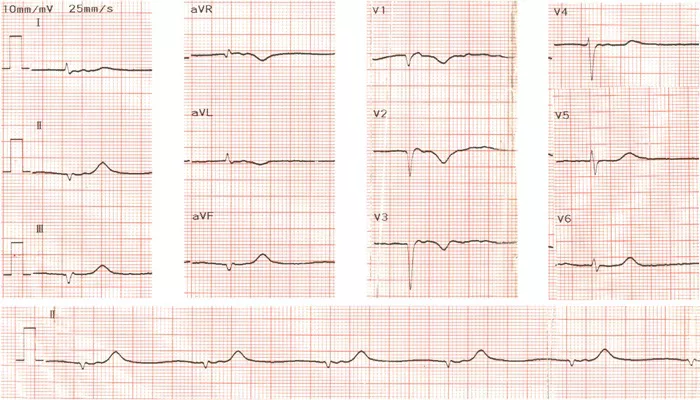
Ventricular bigeminy is a cardiac arrhythmia characterized by the occurrence of a premature ventricular contraction (PVC) following every normal heartbeat, resulting in a repeating pattern of paired beats. This condition can be detected on an electrocardiogram (ECG) as alternating normal and premature beats. While ventricular bigeminy is often benign, its clinical significance and urgency depend on the underlying cardiac status and symptomatology of the patient.
Introduction to Ventricular Bigeminy
Ventricular bigeminy arises when the heart’s normal rhythm is interrupted by an ectopic beat originating in the ventricles.
This premature beat occurs earlier than expected in the cardiac cycle, followed by a compensatory pause before the next normal beat. The pattern resembles a “twin” beat sequence, hence the term “bigeminy” (from Latin bi- meaning two, and gemini meaning twins).
Patients may experience palpitations, a sensation of skipped or extra beats, dizziness, or fatigue. However, many individuals remain asymptomatic, and the arrhythmia is often discovered incidentally during routine ECG monitoring or Holter monitoring.
Pathophysiology and Mechanism
The premature ventricular contractions in bigeminy disrupt the normal electrical conduction and mechanical contraction of the heart. After a PVC, there is a compensatory pause that allows the heart’s electrical system to reset. This pause can lead to dyssynchrony in ventricular contraction and reduced cardiac efficiency. Over time, frequent PVCs, such as those seen in ventricular bigeminy, may contribute to the development of cardiomyopathy by impairing left ventricular function, as evidenced by decreased left ventricular ejection fraction (LVEF) and increased ventricular dimensions.
The mechanism often involves re-entrant circuits within the ventricular myocardium, where the premature beat occurs at a consistent interval after the normal beat, suggesting a re-entrant rather than spontaneous origin.
Clinical Presentation and Diagnosis
Symptoms
- Palpitations or fluttering sensation in the chest
- Feeling of skipped beats or irregular heartbeat
- Dizziness or lightheadedness
- Fatigue or reduced exercise tolerance
- In severe cases, syncope (fainting) may occur
Many patients, however, remain asymptomatic and are diagnosed during cardiac evaluation for other reasons.
Diagnostic Evaluation
Diagnosis is primarily made by ECG, which shows the characteristic pattern of alternating normal and premature ventricular beats. If the arrhythmia is intermittent, extended monitoring with a Holter or event monitor may be necessary to capture the episodes.
Physical examination may reveal irregular heart rhythm, and additional tests such as echocardiography are important to assess cardiac structure and function, especially to rule out underlying heart disease or cardiomyopathy.
Is Ventricular Bigeminy an Emergency?
When It Is Not an Emergency
In patients without structural heart disease and who are asymptomatic, ventricular bigeminy is generally not considered an emergency. It is often benign and may not require treatment beyond lifestyle modifications such as reducing caffeine, alcohol intake, and managing stress.
When It May Be an Emergency
Ventricular bigeminy can become a medical emergency in certain contexts:
Symptomatic patients with hemodynamic instability: If bigeminy causes significant dizziness, syncope, or signs of heart failure, urgent evaluation is warranted.
Underlying structural heart disease: Patients with ischemic heart disease, cardiomyopathy, or heart failure are at higher risk of malignant arrhythmias triggered by frequent PVCs.
High PVC burden: Frequent PVCs can lead to PVC-induced cardiomyopathy, worsening cardiac function and increasing the risk of sustained ventricular tachycardia or fibrillation.
Associated symptoms: Lightheadedness, chest pain, or syncope accompanying bigeminy require prompt medical attention.
In these cases, ventricular bigeminy may herald more serious arrhythmias and necessitate urgent intervention.
Management of Ventricular Bigeminy
Lifestyle and Observation
For asymptomatic patients without heart disease, reassurance and lifestyle changes are often sufficient. Avoidance of stimulants such as caffeine and alcohol, stress management, and correction of electrolyte imbalances can reduce PVC frequency.
Medical Treatment
Symptomatic patients or those with underlying heart disease may benefit from pharmacologic therapy:
Beta-blockers: These are first-line agents to suppress ventricular ectopy and reduce symptoms.
Antiarrhythmic drugs: Class I and III agents are generally avoided due to proarrhythmic risks but may be considered in select cases.
Interventional Treatment
Catheter ablation is an effective treatment for patients with symptomatic ventricular bigeminy refractory to medical therapy or those with PVC-induced cardiomyopathy. Ablation targets the ectopic focus causing the PVCs, often resulting in symptom resolution and improvement in cardiac function.
Prognosis
The prognosis of ventricular bigeminy depends largely on the presence or absence of underlying heart disease and the PVC burden. In healthy individuals, it is usually benign with an excellent prognosis. However, in patients with structural heart disease or high PVC burden, ventricular bigeminy can lead to progressive cardiac dysfunction and increased risk of life-threatening arrhythmias.
Conclusion
Ventricular bigeminy is a common arrhythmia characterized by a premature ventricular contraction following every normal heartbeat. While often benign and asymptomatic, it can be a marker of underlying cardiac pathology or lead to cardiomyopathy if frequent. It is not typically an emergency in healthy individuals but requires urgent evaluation and management when associated with symptoms, hemodynamic compromise, or structural heart disease. Proper diagnosis, risk stratification, and tailored treatment are essential to optimize outcomes in patients with ventricular bigeminy.
Related topics: