Myocardial inflammation, commonly known as myocarditis, is a serious condition characterized by inflammation of the heart muscle. While myocarditis is primarily associated with cardiovascular symptoms such as chest pain, fatigue, and shortness of breath, it can also lead to respiratory symptoms, including cough. This article examines the relationship between myocardial inflammation and cough, exploring the mechanisms behind this connection, the clinical implications, and the importance of recognizing cough as a potential symptom of myocarditis.
Understanding Myocardial Inflammation
What is Myocarditis?
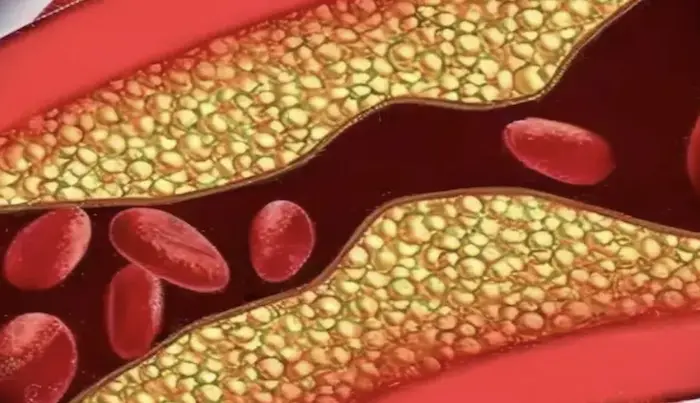
Myocarditis is an inflammatory condition affecting the myocardium, the muscular layer of the heart. This inflammation can result from various causes, including viral infections, autoimmune diseases, and exposure to toxins. The inflammation can disrupt the heart’s ability to pump blood effectively, leading to a range of symptoms and complications.
Types of Myocarditis
Infectious Myocarditis: This is the most common type and is usually caused by viral infections. Common viruses include:
Coxsackievirus
Adenovirus
Influenza virus
SARS-CoV-2 (the virus responsible for COVID-19)
Autoimmune Myocarditis: In this type, the body’s immune system mistakenly attacks the heart muscle. Conditions such as systemic lupus erythematosus (SLE) and rheumatoid arthritis can lead to autoimmune myocarditis.
Toxic Myocarditis: Exposure to certain toxins, including alcohol, heavy metals, and some medications, can result in myocardial inflammation.
Allergic Myocarditis: Some individuals may experience myocarditis as a reaction to specific drugs or allergens.
Causes of Myocardial Inflammation
Understanding the various causes of myocardial inflammation is essential for both prevention and effective management. The primary causes include:
Viral Infections
Viral infections are the leading cause of myocarditis. The immune response to these infections can lead to inflammation in the heart muscle. The viruses can invade the heart directly or trigger an autoimmune response that damages the heart tissue.
Autoimmune Disorders
In autoimmune diseases, the immune system attacks its tissues, including the heart muscle. Conditions such as lupus, rheumatoid arthritis, and sarcoidosis can lead to myocarditis.
Environmental Factors
Exposure to certain environmental toxins, such as heavy metals (lead, mercury) and chemicals (solvents, pesticides), can contribute to myocardial inflammation.
Medications
Some medications can trigger allergic reactions or toxic effects on the heart, leading to inflammation. Examples include certain antibiotics, antipsychotics, and chemotherapeutic agents.
Other Conditions
Other conditions such as ischemic heart disease, chronic kidney disease, and certain infections (e.g., Lyme disease, Chagas disease) can also contribute to the development of myocarditis.
Symptoms of Myocardial Inflammation
The symptoms of myocardial inflammation can vary widely, ranging from mild to severe. Common symptoms include:
Fatigue
Patients often report extreme fatigue, which may be disproportionate to their level of activity.
Shortness of Breath
Dyspnea can occur, especially during exertion or when lying flat (orthopnea). This symptom is due to fluid accumulation in the lungs as a result of heart failure.
Chest Pain
Some patients may experience chest pain or discomfort, which can mimic that of a heart attack. This pain may be sharp or pressure-like.
Palpitations
Irregular heartbeats or a racing heart can occur due to electrical disturbances in the heart caused by inflammation.
Swelling
Peripheral edema (swelling in the legs, ankles, and feet) may occur due to fluid retention as a result of heart failure.
Fever and Flu-like Symptoms
In cases of infectious myocarditis, patients may present with fever, body aches, and other flu-like symptoms.
The Connection Between Myocardial Inflammation and Cough
Mechanisms of Cough in Myocarditis
Cough is not a classic symptom of myocarditis; however, there are several mechanisms through which myocardial inflammation can contribute to coughing:
Heart Failure and Pulmonary Congestion
One of the most significant complications of myocarditis is heart failure. When the heart is unable to pump effectively, blood can back up in the lungs, leading to pulmonary congestion. This congestion can cause fluid to accumulate in the lung tissue and airways, triggering a cough reflex. The cough may be dry or productive, depending on the degree of fluid accumulation.
Inflammatory Response
The inflammatory processes associated with myocarditis can also impact the respiratory system. Inflammation can lead to increased sensitivity of the airways and lung tissues, resulting in a cough. This is particularly relevant in cases where viral infections cause both myocarditis and respiratory symptoms.
Medication Side Effects
Patients with myocarditis may be prescribed various medications to manage their condition, including diuretics and ACE inhibitors. Some of these medications can have side effects that include cough. For example, ACE inhibitors can cause a persistent dry cough in some individuals due to the accumulation of bradykinin, a peptide that promotes inflammation.
Clinical Implications of Cough in Myocarditis
Recognizing cough as a potential symptom of myocarditis is crucial for healthcare providers. A cough in a patient with suspected myocarditis may indicate worsening heart failure or pulmonary congestion, necessitating further evaluation and management. Additionally, a cough may signal the need to reassess the patient’s medication regimen, particularly if the cough is related to medication side effects.
Diagnosis of Myocardial Inflammation
Diagnosing myocardial inflammation involves a combination of clinical evaluation, laboratory tests, imaging studies, and sometimes invasive procedures.
Clinical Evaluation
A thorough medical history and physical examination are crucial. Physicians will inquire about recent infections, symptoms, and family history of heart disease. The presence of a cough, especially if accompanied by other symptoms like shortness of breath or fatigue, should be noted.
Laboratory Tests
Cardiac Biomarkers: Elevated levels of troponin and brain natriuretic peptide (BNP) can indicate myocardial injury and heart failure.
Complete Blood Count (CBC): This may reveal signs of infection or inflammation.
Autoimmune Panels: Tests to check for autoimmune diseases may be performed if suspected.
Electrocardiogram (ECG)
An ECG helps assess the heart’s electrical activity. Changes may indicate myocardial injury, arrhythmias, or other cardiac abnormalities.
Imaging Studies
Echocardiography: This ultrasound of the heart can help assess heart function and structure, revealing any abnormalities in wall motion or chamber size.
Cardiac MRI: This imaging modality is particularly useful for visualizing myocardial inflammation and edema, providing a detailed picture of the heart’s condition.
Endomyocardial Biopsy
In certain cases, a biopsy may be performed to obtain a tissue sample from the heart, allowing for definitive diagnosis of myocarditis.
Treatment Options for Myocardial Inflammation
The treatment of myocardial inflammation focuses on addressing the underlying cause, managing symptoms, and preventing complications. Treatment strategies may include:
Supportive Care
Supportive care is crucial for managing symptoms and monitoring the patient’s condition. This may involve:
Monitoring Vital Signs: Regular monitoring of heart rate, blood pressure, and oxygen saturation.
Fluid Management: Careful management of fluids to prevent overload, particularly in patients with heart failure.
Medications
Anti-inflammatory Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) may be used to reduce inflammation and alleviate pain.
Corticosteroids: In cases of autoimmune myocarditis, corticosteroids may be prescribed to suppress the immune response.
Heart Failure Medications: Medications such as ACE inhibitors, beta-blockers, and diuretics may be used to manage heart failure symptoms and improve cardiac function.
Antivirals: In cases of viral myocarditis, antiviral medications may be considered, although their effectiveness varies.
Management of Arrhythmias
Patients with arrhythmias may require antiarrhythmic medications or interventions such as:
Cardioversion: For patients with unstable tachyarrhythmias.
Implantable Cardioverter-Defibrillator (ICD): In cases of life-threatening arrhythmias or severe left ventricular dysfunction.
Advanced Therapies
For patients with severe myocarditis leading to acute heart failure, advanced therapies may be necessary:
Mechanical Circulatory Support: Devices such as intra-aortic balloon pumps (IABP) or ventricular assist devices (VAD) may be used to support circulation.
Heart Transplantation: In cases of end-stage heart failure refractory to medical therapy, heart transplantation may be considered.
Living with Myocardial Inflammation: Key Considerations
Prognosis and Recovery
The prognosis for individuals with myocardial inflammation varies widely based on several factors:
Severity of the Condition: Patients with mild myocarditis may recover completely, while those with severe inflammation may experience long-term complications.
Underlying Causes: Viral myocarditis often has a better prognosis than autoimmune myocarditis. Identifying and treating the underlying cause is crucial for recovery.
Timeliness of Treatment: Early diagnosis and intervention can significantly improve outcomes.
Long-Term Management
Living with myocardial inflammation often requires ongoing management and monitoring. This may include:
Regular Follow-Up Appointments: Patients should have regular check-ups with their healthcare provider to monitor heart function and adjust treatment as necessary.
Adherence to Medications: Taking prescribed medications consistently is vital for managing symptoms and preventing complications.
Lifestyle Modifications: Patients may need to make lifestyle changes to support heart health, including dietary adjustments, regular exercise, and stress management.
Quality of Life
Many individuals with myocarditis can lead fulfilling lives with appropriate management. Some key aspects of maintaining quality of life include:
Physical Activity: While some patients may need to limit physical exertion, many can engage in moderate exercise as tolerated. It is essential to consult with a healthcare provider before starting any exercise program.
Mental Health Support: Living with a chronic condition can take a toll on mental health. Seeking support from mental health professionals or support groups can be beneficial.
Education and Awareness: Understanding the condition, its symptoms, and treatment options empowers patients to take an active role in their healthcare.
Emergency Preparedness
Patients with a history of myocarditis should be aware of potential warning signs of worsening heart function, such as:
Increased Shortness of Breath: Especially if it worsens with activity or when lying down.
Chest Pain: New or worsening chest pain should be evaluated promptly.
Rapid or Irregular Heartbeat: Any new or concerning changes in heart rhythm should be reported to a healthcare provider.
Lifestyle Modifications to Support Heart Health
In addition to medical treatment, certain lifestyle modifications can support recovery from myocardial inflammation and improve overall heart health:
Diet
Heart-Healthy Diet: A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can support cardiovascular health. Reducing salt intake can help manage blood pressure and fluid retention.
Limit Processed Foods: Avoiding processed foods high in sodium, sugar, and unhealthy fats can improve heart health.
Physical Activity
Gradual Resumption of Activity: Patients should gradually resume physical activity as tolerated, under the guidance of their healthcare provider. Regular, moderate exercise can improve cardiovascular fitness and overall well-being.
Incorporate Daily Movement: Simple activities like walking, stretching, and light household chores can contribute to physical health.
Smoking Cessation
Avoiding Tobacco: Quitting smoking is crucial for heart health. Smoking can exacerbate cardiovascular problems and hinder recovery.
Stress Management
Coping Strategies: Managing stress through relaxation techniques, mindfulness, and counseling can help improve overall health and well-being.
Regular Follow-Up
Ongoing Monitoring: Regular follow-up appointments with a healthcare provider are essential for monitoring heart function and managing any ongoing symptoms.
Conclusion
Myocardial inflammation, or myocarditis, can manifest in various ways, including respiratory symptoms such as cough.
While cough is not a classic symptom of myocarditis, it can occur as a result of pulmonary congestion due to heart failure or as a side effect of medications used to treat the condition. Recognizing cough as a potential symptom of myocarditis is crucial for timely diagnosis and management. For individuals living with myocarditis, awareness of the potential for cough and other respiratory symptoms is essential. With appropriate care and support, many individuals can lead fulfilling lives while managing their condition. The journey may be complex, but with determination and the right resources, it is possible to navigate the challenges posed by myocardial inflammation and maintain a good quality of life.
Related Topics: