Myocardial infarction (MI), commonly known as a heart attack, is a critical medical emergency that occurs when blood flow to a section of the heart is obstructed, leading to damage of the heart muscle. While the classic symptoms of myocardial infarction include chest pain, shortness of breath, and sweating, one less commonly discussed symptom is fever. This article explores the relationship between myocardial infarction and fever, examining the underlying mechanisms, clinical implications, diagnostic considerations, and treatment options.
Understanding Myocardial Infarction
What is Myocardial Infarction?
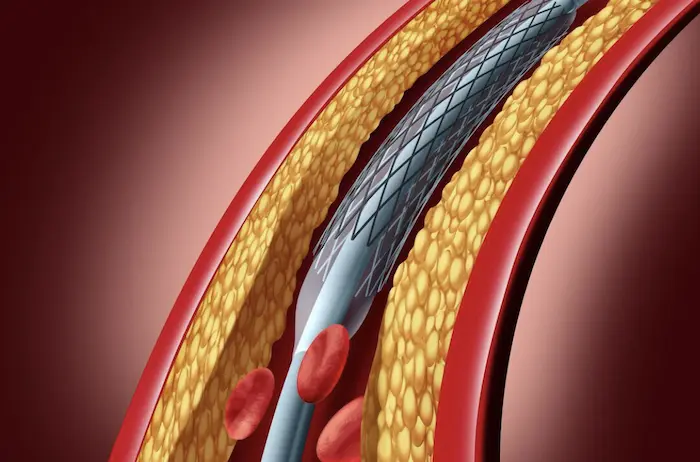
Myocardial infarction occurs when the blood supply to a part of the heart muscle is interrupted, usually due to a blockage in a coronary artery. This blockage can result from atherosclerosis, where fatty deposits build up in the arteries, or from a blood clot that forms on a ruptured plaque. The severity of the infarction depends on the location of the blockage and the duration of ischemia (lack of blood flow).
Symptoms of Myocardial Infarction
The symptoms of myocardial infarction can vary widely among individuals but typically include:
Chest Pain or Discomfort: Often described as a feeling of pressure, squeezing, or fullness in the chest.
Radiating Pain: Pain may radiate to the shoulders, neck, arms, back, teeth, or jaw.
Shortness of Breath: This may occur with or without chest discomfort.
Nausea or Vomiting: Some individuals may experience gastrointestinal symptoms.
Cold Sweat: A sudden onset of sweating (diaphoresis) may occur.
Risk Factors for Myocardial Infarction
Several risk factors contribute to the likelihood of experiencing a myocardial infarction, including:
Age: Risk increases with age, particularly for men over 45 and women over 55.
Family History: A family history of heart disease increases risk.
Smoking: Tobacco use is a major risk factor.
High Blood Pressure: Hypertension can damage arteries over time.
High Cholesterol: Elevated levels of LDL cholesterol can lead to atherosclerosis.
Diabetes: Diabetes significantly increases the risk of coronary artery disease.
Obesity: Excess body weight can lead to various cardiovascular risks.
Sedentary Lifestyle: Lack of physical activity contributes to several risk factors.
Understanding Fever
What is Fever?
Fever is defined as an elevation in body temperature, typically above the normal range of approximately 98.6°F (37°C). It is a common physiological response to infection, inflammation, or other pathological processes. The hypothalamus in the brain regulates body temperature, and a fever occurs when the set point is raised in response to various stimuli.
Causes of Fever
Fever can arise from a variety of causes, including:
Infections: The most common cause of fever, including bacterial, viral, fungal, and parasitic infections.
Inflammatory Conditions: Conditions such as rheumatoid arthritis or inflammatory bowel disease can cause fever due to systemic inflammation.
Malignancies: Certain cancers can lead to fever as a paraneoplastic syndrome.
Medications: Some drugs can cause drug-induced fever as a side effect.
Tissue Injury: Trauma, surgery, or myocardial infarction can trigger a fever response.
The Connection Between Myocardial Infarction and Fever
Mechanisms Leading to Fever After Myocardial Infarction
The relationship between myocardial infarction and fever is complex and can be attributed to several mechanisms:
Inflammatory Response
One of the primary reasons myocardial infarction can lead to fever is the inflammatory response that occurs following tissue injury. When the heart muscle is damaged during an MI, the body activates its immune response, leading to:
Release of Cytokines: Damaged myocardial cells release pro-inflammatory cytokines such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and interleukin-1 beta (IL-1β). These cytokines play a crucial role in the inflammatory process and can act on the hypothalamus to raise the body’s temperature set point, resulting in fever.
Systemic Inflammation: The inflammatory response can lead to a systemic inflammatory response syndrome (SIRS), characterized by fever, increased heart rate, and changes in white blood cell counts.
Infection
Patients who experience myocardial infarction may also develop infections, which can contribute to fever. Possible sources of infection include:
Pneumonia: Patients who are hospitalized after MI may be at risk for developing pneumonia, especially those with reduced mobility or respiratory complications.
Urinary Tract Infections (UTIs): Hospitalized patients are also at risk for UTIs, which can present with fever.
Endocarditis: Although rare, infections of the heart valves can occur following myocardial infarction, leading to persistent fever.
Cardiac Complications
Certain complications following myocardial infarction can also lead to fever:
Pericarditis: Inflammation of the pericardium (the membrane surrounding the heart) can occur after an MI, leading to fever and chest pain. This condition is often referred to as post-myocardial infarction pericarditis or Dressler’s syndrome.
Heart Failure: Acute heart failure following MI can lead to pulmonary congestion and respiratory distress, which may be accompanied by fever due to the stress response.
Clinical Implications of Fever Following Myocardial Infarction
The presence of fever in patients with myocardial infarction has several clinical implications:
Indicator of Complications: Fever can be an early indicator of complications such as infections or inflammatory responses, necessitating further evaluation and management.
Impact on Recovery: The presence of fever can affect a patient’s recovery trajectory, potentially prolonging hospitalization and complicating the management of myocardial infarction.
Diagnostic Challenge: Fever can complicate the clinical picture, making it challenging to distinguish between post-MI complications and other underlying conditions. Healthcare providers must carefully evaluate the source of fever in these patients.
Increased Monitoring: Patients with fever following MI may require increased monitoring for vital signs, laboratory tests, and imaging studies to identify the cause of the fever.
Diagnosis of Fever Following Myocardial Infarction
Clinical Assessment
A thorough clinical assessment is essential for diagnosing the cause of fever in patients with myocardial infarction. Key components include:
Patient History: Gathering information about the onset and duration of fever, associated symptoms (e.g., cough, dysuria, chest pain), and any recent hospitalizations or surgeries.
Physical Examination: A physical exam may reveal signs of infection (e.g., lung auscultation for crackles, abdominal examination for tenderness) or inflammation (e.g., pericardial friction rub).
Diagnostic Tests
Several diagnostic tests can aid in identifying the cause of fever:
Blood Tests: Laboratory tests can help identify signs of infection or inflammation, including:
Complete Blood Count (CBC): Elevated white blood cell count may indicate infection.
C-reactive Protein (CRP): Elevated levels of CRP can indicate systemic inflammation.
Blood Cultures: If an infection is suspected, blood cultures can help identify the causative organism.
Imaging Studies: Imaging studies may be necessary to evaluate for complications such as pneumonia or pericarditis:
Chest X-Ray: Can reveal signs of pneumonia or pleural effusion.
Echocardiography: Useful for assessing cardiac function and evaluating for pericardial effusion or other structural complications.
Urinalysis: A urinalysis may be performed to assess for urinary tract infections, especially in hospitalized patients.
Treatment of Fever Following Myocardial Infarction
Immediate Management
The immediate management of fever in the context of myocardial infarction focuses on identifying and addressing the underlying cause. Key interventions include:
Antipyretics: Medications such as acetaminophen or ibuprofen may be used to reduce fever and alleviate discomfort.
Antibiotics: If an infection is suspected, appropriate antibiotics should be initiated based on clinical judgment and local guidelines.
Supportive Care: Ensuring adequate hydration and comfort measures can help manage fever and its associated symptoms.
Long-Term Management
Long-term management of fever following myocardial infarction involves addressing the underlying heart condition and preventing future complications:
Medications: Patients may be prescribed a combination of medications to manage heart function and prevent further ischemic events:
Antiplatelet Agents: Medications such as aspirin or clopidogrel are commonly prescribed to reduce the risk of future heart attacks.
Beta-Blockers: These medications help decrease heart rate and myocardial oxygen demand.
ACE Inhibitors: Used to reduce afterload and improve cardiac output.
Lifestyle Modifications: Patients should be encouraged to adopt heart-healthy lifestyle changes, including:
Dietary Changes: A low-sodium, heart-healthy diet can help manage blood pressure and reduce the risk of heart disease.
Regular Exercise: Engaging in regular physical activity, as tolerated, can improve cardiovascular health.
Smoking Cessation: Quitting smoking is crucial for reducing cardiovascular risk.
Cardiac Rehabilitation: Participation in a structured cardiac rehabilitation program can help patients recover and improve their overall cardiovascular health.
Monitoring and Follow-Up: Regular follow-up appointments are essential for monitoring heart function and adjusting medications as needed. Patients should be educated about recognizing early signs of complications.
Prevention of Fever Following Myocardial Infarction
Preventing fever in patients with myocardial infarction involves managing risk factors and promoting heart health. Key strategies include:
Early Recognition and Treatment of Myocardial Infarction: Prompt recognition and treatment of MI can minimize heart damage and reduce the risk of complications such as fever.
Management of Comorbidities: Effective management of conditions such as hypertension, diabetes, and hyperlipidemia can reduce the risk of myocardial infarction and subsequent complications.
Adherence to Medications: Patients should be encouraged to adhere to prescribed medications to manage heart failure and prevent fluid overload.
Education and Awareness: Educating patients about the signs and symptoms of heart failure and fever can empower them to seek timely medical attention.
Regular Health Check-Ups: Routine check-ups with healthcare providers can help monitor cardiovascular health and identify potential issues before they become severe.
Conclusion
Myocardial infarction is a serious condition that can lead to a range of complications, including fever. The relationship between these two conditions is primarily mediated through the inflammatory response, potential infections, and cardiac complications. Understanding this connection is crucial for timely diagnosis and effective management.
Patients who develop fever following myocardial infarction require immediate medical attention and comprehensive management strategies to address both the fever and the underlying heart condition. Long-term management involves a combination of medications, lifestyle modifications, and regular follow-up to prevent future events and improve overall quality of life.
Related Topics: