Myocardial inflammation, commonly referred to as myocarditis, is a serious condition characterized by inflammation of the heart muscle (myocardium). This inflammation can lead to a range of complications, including heart failure, arrhythmias, and even sudden cardiac death. The life-threatening nature of myocarditis is often underestimated, as many patients may initially present with nonspecific symptoms that mimic less severe conditions. In this article, we will explore the reasons why myocardial inflammation is life-threatening, the underlying mechanisms, the clinical presentation, diagnostic challenges, and treatment options.
Understanding Myocardial Inflammation
Definition and Pathophysiology
Myocarditis is defined as inflammation of the myocardium, which can impair the heart’s ability to pump blood effectively.
The inflammation can be caused by various factors, including:
Infectious Agents: Viral infections are the most common cause of myocarditis, with viruses such as Coxsackievirus, adenovirus, and, more recently, SARS-CoV-2 being implicated. Bacterial and fungal infections can also contribute.
Autoimmune Conditions: Diseases such as systemic lupus erythematosus, rheumatoid arthritis, and sarcoidosis can lead to myocarditis through autoimmune mechanisms.
Toxic Exposures: Certain drugs, alcohol, and environmental toxins can induce myocardial inflammation.
Idiopathic Cases: In many instances, the exact cause of myocarditis remains unknown.
The pathophysiology of myocarditis involves an initial insult that triggers an inflammatory response. This response can lead to direct damage to cardiac myocytes, resulting in impaired contractility and heart function.
Mechanisms of Injury
The mechanisms by which myocardial inflammation leads to cardiac injury include:
Direct Viral Injury: Certain viruses can directly invade cardiac myocytes, leading to cell death and inflammation.
Immune-Mediated Damage: The immune response to infection or injury can lead to the infiltration of inflammatory cells, such as lymphocytes and macrophages, which release cytokines and other mediators that exacerbate tissue damage.
Endothelial Dysfunction: Inflammation can lead to endothelial cell injury, increasing vascular permeability and contributing to myocardial edema.
Microvascular Dysfunction: Inflammation can impair blood flow to the myocardium, leading to ischemia and further injury.
Clinical Presentation of Myocardial Inflammation
Symptoms
The clinical presentation of myocarditis can vary widely, but common symptoms include:
Chest Pain: Often sharp or pressure-like, mimicking angina or myocardial infarction.
Shortness of Breath: Dyspnea on exertion or at rest, which may be due to heart failure or pulmonary congestion.
Fatigue: Unexplained fatigue that may worsen with activity.
Palpitations: Irregular heartbeats or a sensation of a racing heart.
Flu-like Symptoms: Fever, myalgia, and malaise, particularly in cases of viral myocarditis.
Signs of Heart Failure
As myocarditis progresses, patients may develop signs of heart failure, including:
Jugular Venous Distension: Increased pressure in the jugular veins due to elevated central venous pressure.
Pulmonary Crackles: Rales heard on auscultation due to pulmonary congestion.
Peripheral Edema: Swelling in the legs and feet due to fluid retention.
Decreased Exercise Tolerance: Difficulty with physical activity due to reduced cardiac output.
Arrhythmias
Myocarditis can also lead to arrhythmias, which can be life-threatening. Common arrhythmias associated with myocarditis include:
Atrial Fibrillation: Irregular and often rapid heart rate that can lead to ineffective blood pumping.
Ventricular Tachycardia: A fast heart rate originating from the ventricles, which can compromise cardiac output and lead to syncope or sudden cardiac arrest.
Ventricular Fibrillation: A chaotic electrical activity in the heart that can lead to sudden cardiac death if not treated immediately.
Why Is Myocardial Inflammation Life-Threatening?
Risk of Heart Failure
One of the most significant risks associated with myocarditis is the development of heart failure. The inflammatory process can lead to:
Reduced Contractility: Inflammation and injury to cardiac myocytes can impair the heart’s ability to contract effectively, leading to decreased cardiac output.
Diastolic Dysfunction: Inflammation can lead to stiffness of the myocardium, impairing the heart’s ability to fill properly during diastole.
Fluid Overload: As heart function declines, fluid can accumulate in the lungs and peripheral tissues, leading to pulmonary congestion and edema.
Heart failure resulting from myocarditis can be acute or chronic, and it may require aggressive management, including hospitalization, diuretics, and in severe cases, mechanical support or transplantation.
Risk of Arrhythmias
The presence of inflammation in the myocardium can disrupt the normal electrical conduction system of the heart, leading to arrhythmias. Arrhythmias can be life-threatening for several reasons:
Reduced Cardiac Output: Fast or irregular heart rhythms can significantly reduce the heart’s ability to pump blood effectively, leading to hypotension and inadequate perfusion of vital organs.
Risk of Sudden Cardiac Death: Certain arrhythmias, particularly ventricular tachycardia and ventricular fibrillation, can lead to sudden cardiac arrest if not treated promptly.
Increased Risk of Thromboembolism: Atrial fibrillation, a common arrhythmia in myocarditis, increases the risk of thrombus formation in the left atrium, which can lead to stroke.
Risk of Ischemia
Myocarditis can lead to microvascular dysfunction, impairing blood flow to the myocardium. This can result in ischemia, which can exacerbate myocardial injury and contribute to heart failure and arrhythmias. Ischemia can also lead to:
Infarction: Prolonged ischemia can result in myocardial infarction, further compromising heart function.
Increased Troponin Levels: Ischemia can lead to elevated troponin levels, which can complicate the clinical picture and delay diagnosis.
Autoimmune Responses
In cases of autoimmune myocarditis, the inflammatory response may not only target the myocardium but also other organs.
This systemic involvement can lead to:
Multi-Organ Dysfunction: Severe autoimmune responses can affect the lungs, kidneys, and liver, leading to multi-organ failure.
Increased Mortality: Patients with autoimmune myocarditis may have a higher risk of mortality due to the systemic nature of the disease.
Delayed Diagnosis and Treatment
The nonspecific symptoms of myocarditis can lead to delays in diagnosis and treatment. This is particularly concerning because:
Misdiagnosis: Patients may be misdiagnosed with less severe conditions, delaying appropriate management.
Worsening Condition: Delayed recognition of myocarditis can lead to progression of the disease, increasing the risk of complications, including heart failure and arrhythmias.
Diagnostic Challenges
Clinical Evaluation
A thorough clinical evaluation is essential for diagnosing myocarditis. Key components include:
History and Physical Examination: A detailed history of symptoms, recent infections, and autoimmune conditions is crucial. Physical examination may reveal signs of heart failure and arrhythmias.
Electrocardiogram (ECG): An ECG can reveal arrhythmias, ST segment changes, and other abnormalities associated with myocarditis.
Biomarkers
Troponin Levels: Elevated troponin levels can indicate myocardial injury, but they are not specific to myocarditis. Other conditions, such as myocardial infarction, can also cause elevated troponin levels.
B-type Natriuretic Peptide (BNP): Elevated levels of BNP can indicate heart failure, but they do not specifically diagnose myocarditis.
Imaging Studies
Imaging studies can provide valuable information in the diagnosis and assessment of myocarditis:
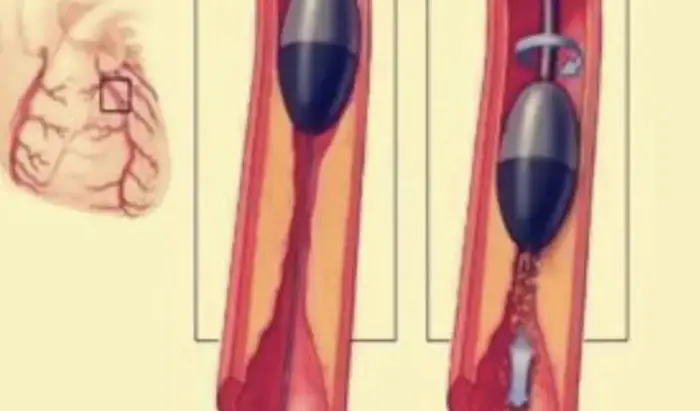
Echocardiography: This non-invasive imaging technique can assess cardiac function and identify wall motion abnormalities. It may also reveal complications such as left ventricular thrombus.
Cardiac Magnetic Resonance Imaging (MRI): Cardiac MRI is considered the gold standard for diagnosing myocarditis. It can assess myocardial inflammation, edema, and fibrosis, providing a comprehensive evaluation of cardiac involvement.
Endomyocardial Biopsy
In certain cases, an endomyocardial biopsy may be performed to obtain tissue samples for histological examination. This invasive procedure is typically reserved for cases where the diagnosis is uncertain or when specific treatment is being considered, such as in cases of suspected autoimmune myocarditis.
Treatment of Myocardial Inflammation
Initial Management
The management of myocarditis is primarily supportive and focuses on addressing symptoms and preventing complications. Key components of initial management include:
Hospitalization: Patients with severe symptoms, heart failure, or arrhythmias may require hospitalization for monitoring and treatment.
Heart Failure Management: Standard heart failure management strategies, including the use of diuretics, ACE inhibitors, and beta-blockers, may be employed to alleviate symptoms and improve cardiac function.
Anti-inflammatory Therapy: In cases of autoimmune myocarditis, immunosuppressive agents such as corticosteroids or other immunomodulatory therapies may be indicated.
Antiviral Therapy: In cases of viral myocarditis, specific antiviral therapy may be considered, although evidence supporting this is limited.
Long-Term Management
Long-term management of myocarditis focuses on preventing recurrence and optimizing cardiovascular health:
Cardiac Rehabilitation: A structured cardiac rehabilitation program can help patients recover physically and emotionally after an episode of myocarditis. It includes exercise training, education on heart-healthy living, and counseling.
Lifestyle Modifications: Patients should be encouraged to adopt a heart-healthy lifestyle, including a balanced diet, regular physical activity, smoking cessation, and weight management.
Medication Adherence: Long-term medications, including antiplatelet agents, beta-blockers, ACE inhibitors, and statins, should be prescribed to reduce the risk of future cardiovascular events.
Regular Follow-Up: Patients should have regular follow-up appointments with their healthcare provider to monitor their cardiovascular health and adjust treatment as needed.
Conclusion
Myocardial inflammation is a life-threatening condition due to its potential to cause heart failure, arrhythmias, ischemia, and systemic complications. The nonspecific nature of its symptoms can lead to delayed diagnosis and treatment, exacerbating the risks associated with the condition. Understanding the mechanisms by which myocardial inflammation leads to these serious complications is crucial for clinicians in making timely and effective management decisions.
Early recognition and appropriate management of myocarditis can significantly improve outcomes for affected patients. As research continues to advance our understanding of this complex condition, ongoing efforts to enhance diagnostic accuracy and treatment strategies will be essential in reducing the morbidity and mortality associated with myocardial inflammation.
Related Topics: