Inferior myocardial infarction (MI) is a type of heart attack that affects the inferior (lower) wall of the heart. This condition occurs when blood flow through the right coronary artery (RCA) or, less commonly, the left circumflex artery is blocked, leading to damage or death of the heart muscle in that region. Understanding the symptoms, causes, and treatment options for inferior MI is crucial for timely diagnosis and effective management.
What Is Inferior Myocardial Infarction?
Inferior myocardial infarction is a subset of acute myocardial infarctions characterized by the involvement of the inferior wall of the left ventricle. The inferior wall is primarily supplied by the right coronary artery in about 90-94% of people, while in 6-10% of the population, the left circumflex artery supplies this area due to left coronary dominance. When a blockage occurs in these arteries, the affected heart muscle suffers from ischemia (lack of oxygen), which can progress to infarction (tissue death) if not treated promptly.
Causes of Inferior Myocardial Infarction
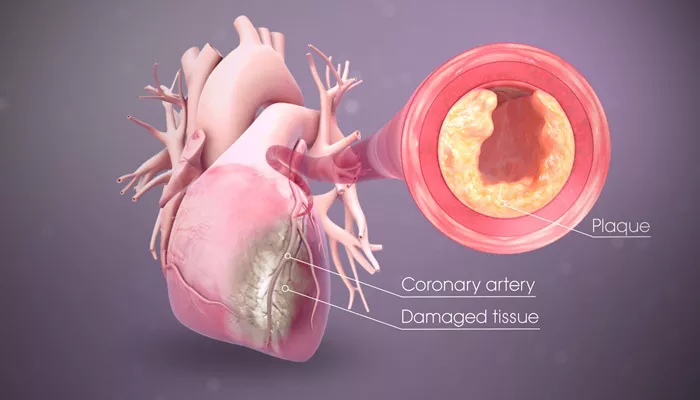
The primary cause of inferior MI is coronary artery disease (CAD), which involves the buildup of atherosclerotic plaques inside the coronary arteries. These plaques are composed of cholesterol, fatty substances, and cellular debris. Over time, plaques can rupture, triggering the formation of a blood clot (thrombus) that suddenly blocks the artery and stops blood flow to the heart muscle.
Other causes include:
Coronary artery spasm: A temporary tightening of the artery muscles can reduce blood flow.
Progressive hemodynamic stenosis: Gradual narrowing of the artery.
Rare causes: Such as ascending aortic dissection involving the right coronary ostium.
Increased oxygen demand: Conditions like fever, rapid heart rate, or anemia can worsen ischemia in already narrowed arteries.
Symptoms of Inferior Myocardial Infarction
Symptoms of inferior MI can vary but often include:
Chest pain or discomfort: Typically retrosternal, described as pressure, squeezing, heaviness, or crushing pain. The pain may radiate to the left arm, neck, jaw, or back.
Shortness of breath: Due to reduced heart function.
Nausea and vomiting: More common in inferior MI due to vagal nerve stimulation.
Sweating and cold clammy skin: Signs of sympathetic nervous system activation.
Bradycardia and heart block: Inferior MI can affect the atrioventricular (AV) node, leading to conduction abnormalities such as first-degree to complete AV block, often with junctional escape rhythms.
Fatigue, dizziness, or fainting: Due to decreased cardiac output and possible hypotension.
Women and older adults may present atypically, with less chest pain and more symptoms like fatigue, nausea, or shortness of breath.
Diagnosis
The diagnosis of inferior MI is primarily based on clinical presentation, electrocardiogram (ECG) findings, and cardiac biomarkers:
ECG: Shows ST-segment elevation in the inferior leads II, III, and aVF. Reciprocal ST depression may be seen in the lateral leads (I, aVL, V5, V6).
Cardiac enzymes: Elevated troponin levels confirm myocardial injury.
Imaging: Echocardiography can assess wall motion abnormalities and complications like right ventricular infarction.
Complications
Inferior MI can lead to several complications, including:
Conduction disturbances: AV block due to ischemia of the AV node.
Right ventricular infarction: Occurs in some cases, causing hypotension and shock.
Arrhythmias: Ventricular tachycardia or fibrillation.
Mechanical complications: Acute mitral valve regurgitation, ventricular septal defect, or left ventricular aneurysm.
Treatment of Inferior Myocardial Infarction
The goals of treatment are to restore blood flow to the affected myocardium, relieve symptoms, prevent complications, and improve long-term outcomes.
Emergency Management
Immediate medical attention: Call emergency services if MI is suspected.
Oxygen therapy: Administered if oxygen saturation is low.
Aspirin: To inhibit platelet aggregation and reduce clot growth.
Nitroglycerin: To relieve chest pain by dilating coronary arteries.
Pain control: Opioids like morphine may be used for severe pain but with caution due to potential side effects.
Reperfusion Therapy
Percutaneous coronary intervention (PCI): The preferred treatment for ST-elevation MI (STEMI), ideally performed within 90 minutes of hospital arrival. PCI involves mechanically opening the blocked artery using a balloon and stent.
Fibrinolytic therapy: Used if PCI is not immediately available, especially within the first few hours of symptom onset.
NSTEMI management: PCI is performed within 24-48 hours for stable patients or immediately for unstable patients.
Medical Therapy
Antiplatelet agents: Dual antiplatelet therapy with aspirin and a P2Y12 inhibitor.
Anticoagulants: To prevent further clot formation.
Beta-blockers: To reduce heart rate and myocardial oxygen demand.
Statins: To stabilize plaques and reduce cholesterol.
ACE inhibitors or ARBs: To improve cardiac remodeling and reduce heart failure risk.
Monitoring and Support
Continuous ECG monitoring for arrhythmias.
Management of bradycardia or heart block with atropine or temporary pacing if needed.
Treatment of complications like heart failure or cardiogenic shock.
Conclusion
Inferior myocardial infarction is a serious cardiac event caused mainly by blockage of the right coronary artery. Prompt recognition of symptoms and immediate treatment are critical to saving heart muscle and lives. Advances in reperfusion therapy and medical management have improved outcomes, but prevention remains key to reducing the burden of this condition.
Related topics: