Calcium channel blockers (CCBs) are a vital class of medications widely used in cardiovascular medicine. These drugs work by inhibiting the entry of calcium ions into the cells of the heart and blood vessel walls. Calcium plays a crucial role in muscle contraction, including the contraction of the heart muscle and the smooth muscles lining arteries. By blocking calcium influx, CCBs cause relaxation of blood vessels and reduce the heart’s workload, leading to lower blood pressure and improved blood flow. This makes them effective in treating several cardiovascular conditions such as hypertension, angina, and certain arrhythmias. This article provides a detailed overview of the types of calcium channel blockers, their clinical uses, and potential side effects.
Types of Calcium Channel Blockers
Calcium channel blockers are broadly divided into two main classes based on their chemical structure and primary site of action:
1. Dihydropyridines (DHPs)
Dihydropyridines primarily act on the smooth muscle cells of blood vessels. They cause vasodilation, which lowers systemic vascular resistance and arterial pressure. This class is especially effective in treating high blood pressure and conditions related to arterial constriction. Common dihydropyridines include:
- Amlodipine
- Nifedipine
- Felodipine
- Nicardipine
- Nimodipine (notable for crossing the blood-brain barrier and used to prevent cerebral vasospasm)
DHPs are often preferred for hypertension because they predominantly dilate arteries without significantly affecting heart rate or contractility. However, they can cause reflex tachycardia due to vasodilation.
2. Non-Dihydropyridines (Non-DHPs)
Non-dihydropyridines affect both the heart and blood vessels. They reduce heart rate and decrease the force of heart muscle contraction, in addition to causing some vasodilation. This makes them useful for treating arrhythmias as well as hypertension and angina. The two main non-DHP drugs are:
- Verapamil (phenylalkylamine class)
- Diltiazem (benzothiazepine class)
These drugs slow down the conduction of electrical impulses in the heart, which helps control abnormal heart rhythms such as atrial fibrillation. They are also used to reduce myocardial oxygen demand by lowering heart rate and contractility.
Uses of Calcium Channel Blockers
Calcium channel blockers have multiple cardiovascular applications, including:
Hypertension (High Blood Pressure)
CCBs are effective antihypertensive agents. By dilating arteries, they reduce peripheral resistance and lower blood pressure.
They are particularly useful in elderly patients with stiff arteries and isolated systolic hypertension. Both DHPs and non-DHPs are used, but DHPs are more commonly prescribed due to their potent vasodilatory effects.
Angina Pectoris (Chest Pain)
CCBs improve oxygen delivery to the heart by dilating coronary arteries and reducing cardiac workload. This helps relieve chest pain caused by reduced blood flow to the heart muscle. Both classes are used; non-DHPs additionally reduce heart rate and contractility, further lowering oxygen demand.
Cardiac Arrhythmias
Non-DHP calcium channel blockers (verapamil and diltiazem) are used to manage supraventricular tachycardias and atrial fibrillation by slowing electrical conduction through the atrioventricular node. This helps control heart rate and restore rhythm.
Other Uses
Nimodipine is used to prevent cerebral vasospasm after subarachnoid hemorrhage.
CCBs may be used off-label for conditions such as Raynaud’s phenomenon, pulmonary hypertension, and migraine prevention.
Research is ongoing into their potential role in delaying neurodegenerative diseases linked to hypertension, such as dementia and Alzheimer’s disease.
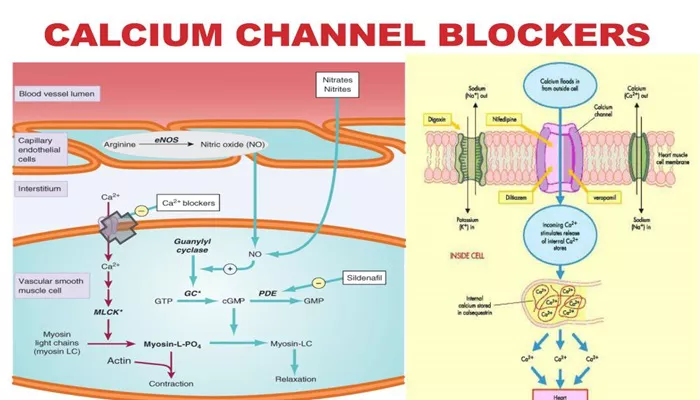
Mechanism of Action
Calcium channel blockers inhibit the L-type voltage-gated calcium channels located in the membranes of cardiac and smooth muscle cells. Normally, calcium influx through these channels triggers muscle contraction. By blocking calcium entry:
Vascular smooth muscle relaxation occurs, causing vasodilation and decreased blood pressure.
Cardiac muscle contraction strength decreases (negative inotropy).
Heart rate slows due to reduced conduction velocity in nodal tissues (negative chronotropy and dromotropy).
Aldosterone production in the adrenal cortex is reduced, contributing to blood pressure lowering.
Side Effects of Calcium Channel Blockers
While generally well tolerated, calcium channel blockers can cause side effects, which vary depending on the drug class and individual patient factors.
Common Side Effects
Dihydropyridines: Flushing, headache, dizziness, peripheral edema (ankle swelling), and reflex tachycardia due to vasodilation.
Non-Dihydropyridines: Constipation (especially verapamil), bradycardia (slow heart rate), dizziness, and fatigue.
Other frequent side effects include nausea, rash, and flushing. Gingival hyperplasia (overgrowth of gums) is a known side effect of many CCBs.
Serious Side Effects and Precautions
Excessive lowering of heart rate or blood pressure, which can cause dizziness or fainting.
Worsening of heart failure symptoms, especially in patients with systolic dysfunction; non-DHPs are generally avoided in such cases.
Potential interactions with other medications that affect heart rate or blood pressure.
Avoid grapefruit or grapefruit juice as it can increase CCB blood levels, leading to toxicity.
Overdose, particularly with verapamil, can be life-threatening due to profound cardiac effects.
Patients should never double doses if a dose is missed, as this can cause dangerous side effects.
Conclusion
Calcium channel blockers are a cornerstone in the management of hypertension, angina, and certain arrhythmias. Their ability to relax blood vessels and modulate heart function makes them versatile and effective. Understanding the differences between dihydropyridine and non-dihydropyridine classes helps clinicians tailor therapy to individual patient needs while minimizing side effects. Despite their benefits, careful dosing and monitoring are essential to avoid adverse effects and drug interactions. With ongoing research, the therapeutic scope of calcium channel blockers may expand further, potentially benefiting patients with neurodegenerative and other chronic diseases.
Related topics: