Atrial fibrillation (AFib) is a common heart rhythm disorder affecting nearly 10% of individuals over 80. While AFib itself isn’t immediately life-threatening, its long-term impact on mortality and quality of life becomes significant, particularly after age 70. Studies show that with proper management, older adults can maintain a positive outlook, though mortality rates remain higher than in those without AFib.
Understanding AFib and Aging
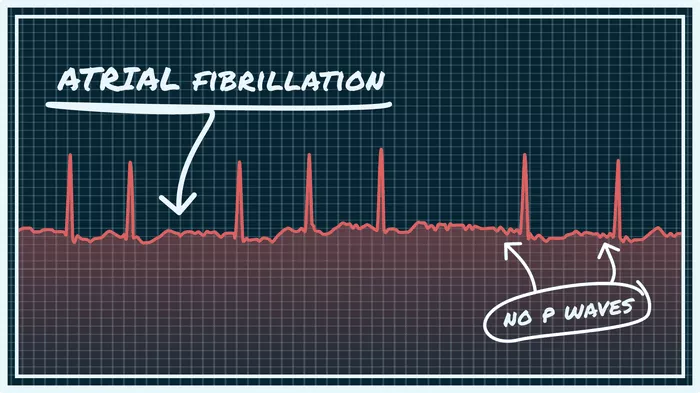
AFib causes irregular heartbeats, increasing stroke and heart failure risks. Aging weakens heart tissue and elevates blood pressure, making AFib more likely. By age 70, the cumulative effects of cardiovascular wear-and-tear and comorbidities like diabetes or hypertension amplify these risks.
Mortality Rates in Older Adults with AFib
Baseline Risk Increase:
A 2020 study found adults over 70 with AFib face twice the mortality rate of peers without AFib. Early diagnosis through screening correlated with a 29% higher mortality risk, likely due to delayed treatment initiation.
Long-Term Survival Data:
15-year survival: 92% for patients with “lone AFib” (no structural heart disease).
30-year survival: Drops to 68%, mirroring age-related declines in the general population.
AFib progression: Each decade after diagnosis raises progression to permanent AFib risk by 70%.
Regional and Demographic Trends:
U.S. data (1999–2019) shows AFib-related deaths in adults ≥75 more than doubled, with women and White individuals disproportionately affected.
Key Factors Influencing Life Expectancy
1. Comorbidities
Non-cardiovascular conditions (e.g., cancer, pneumonia) cause 60% of deaths in elderly AFib patients. Concurrent heart failure or kidney disease further reduces survival.
2. Stroke Prevention
Anticoagulants (e.g., warfarin, DOACs) lower stroke risk by 60–70%, but underuse in older adults remains common due to bleeding concerns.
3. Rhythm vs. Rate Control
Rhythm control: Restoring normal heartbeats via medications or ablation.
Rate control: Slowing heart rate with beta-blockers.
Both strategies show similar long-term outcomes, but personalized plans improve quality of life.
4. Lifestyle Modifications
Weight management: Obesity increases AFib recurrence.
Alcohol reduction: Heavy drinking triggers episodes.
Exercise: Moderate activity improves cardiovascular resilience.
Improving Outcomes After 70
| Strategy | Impact |
| Early Anticoagulation | Reduces stroke risk by 64% |
| Regular Monitoring | Lowers hospitalization rates |
| Comorbidity Management | Slows disease progression |
Medication Adherence: Skipping doses or self-adjusting therapies raises complications. Fixed-dose DOACs simplify regimens.
Fall Prevention: Balance exercises and home safety reduce bleeding risks from anticoagulants.
Advanced Interventions:
Catheter ablation: Effective for symptomatic AFib, even in octogenarians.
Pacemakers: Used if AFib causes dangerous bradycardia.
Causes of Death in Elderly AFib Patients
Cardiovascular (40%):
- Heart failure
- Stroke
- Sudden cardiac death.
Non-Cardiovascular (60%):
- Cancer
- Respiratory infections
- Sepsis.
The Role of Timely Diagnosis
Delayed AFib detection allows blood clots to form, increasing stroke risk. Routine pulse checks and wearable ECG monitors (e.g., smartwatches) enable earlier intervention.
Conclusion
Life expectancy with AFib after 70 depends heavily on proactive care. While mortality rates are higher than in healthier peers, combining anticoagulation, lifestyle changes, and comorbidity management can extend survival and preserve quality of life. Regular cardiology follow-ups and patient education remain critical to mitigating risks.
Related topics: