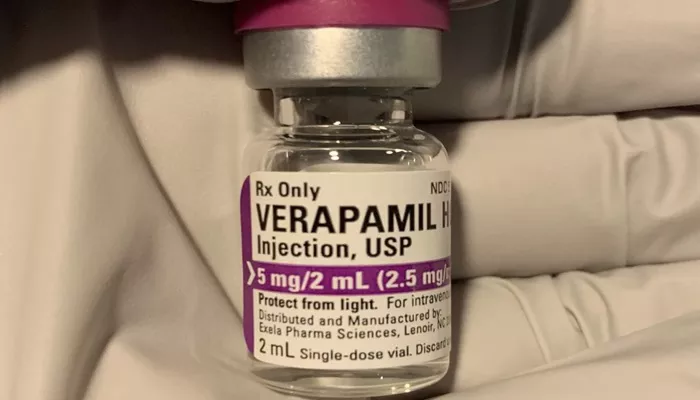
Verapamil is a calcium channel blocker. It is commonly used to treat hypertension, angina, and certain arrhythmias. It works by relaxing blood vessels and slowing the heart rate.
What Is Heart Failure?
Heart failure is a chronic condition. The heart is unable to pump blood effectively. This leads to fatigue, shortness of breath, and fluid retention. Heart failure can be classified as systolic or diastolic.
Why Medication Choice Is Critical
In heart failure, certain drugs may worsen cardiac function. Verapamil is one of these drugs. Understanding why it is contraindicated helps improve patient outcomes.
How Verapamil Works
Mechanism of Action
Verapamil blocks L-type calcium channels. This reduces calcium entry into cardiac and vascular smooth muscle cells. As a result, it decreases myocardial contractility and heart rate.
Cardiovascular Effects
Verapamil reduces oxygen demand and controls heart rhythm. It also dilates arteries. These effects are beneficial in angina and supraventricular tachycardia.
Negative Inotropic Properties
Verapamil weakens the force of heart muscle contractions. This is known as a negative inotropic effect. In heart failure, this effect can be dangerous.
Types of Heart Failure and Their Sensitivity to Verapamil
Systolic Heart Failure
This type involves reduced ejection fraction. The heart cannot pump blood effectively. Verapamil’s negative inotropic action further reduces contractility. This can worsen the condition.
Diastolic Heart Failure
Also called heart failure with preserved ejection fraction. It involves stiff ventricles that do not relax well. Although verapamil may help by slowing the heart rate, it still poses risks due to its effects on conduction and pressure.
Clinical Evidence Against Verapamil in Heart Failure
Research Findings
Studies show that verapamil reduces cardiac output in patients with systolic dysfunction. Clinical trials observed worsening symptoms and increased hospitalization rates.
Comparison With Other Calcium Channel Blockers
Non-dihydropyridine calcium channel blockers like verapamil and diltiazem have strong myocardial effects. In contrast, dihydropyridines like amlodipine are safer in some cases of heart failure.
Guidelines From Major Cardiology Associations
The American Heart Association and the European Society of Cardiology recommend avoiding verapamil in patients with reduced ejection fraction. This is based on strong clinical data.
Why Is Verapamil Contraindicated in Heart Failure
Worsening of Symptoms
Patients may experience increased shortness of breath, swelling, and fatigue. Verapamil reduces contractility, limiting the heart’s ability to respond to stress.
Bradycardia and Heart Block
Verapamil slows AV node conduction. In heart failure, this can lead to severe bradycardia or complete heart block, especially if combined with beta-blockers.
Hypotension
Verapamil causes vasodilation. In heart failure, this can result in dangerously low blood pressure, reducing organ perfusion and causing dizziness or fainting.
Fluid Retention and Pulmonary Edema
Verapamil’s negative inotropic effects may promote fluid retention. This can cause or worsen pulmonary congestion, a hallmark of decompensated heart failure.
Exceptions and Special Considerations
Hypertrophic Cardiomyopathy
In selected patients with hypertrophic obstructive cardiomyopathy, verapamil may be used carefully. It helps reduce outflow tract obstruction by slowing the heart rate.
Rate Control in Atrial Fibrillation
For patients with diastolic dysfunction and atrial fibrillation, low-dose verapamil may be considered under strict supervision. Still, beta-blockers are usually preferred.
Close Monitoring Required
If verapamil must be used, regular monitoring of heart rate, blood pressure, and ejection fraction is necessary. Hospital-based initiation is often advised.
Safer Alternatives for Heart Failure Patients
Beta-Blockers
Drugs like carvedilol, metoprolol, and bisoprolol are first-line therapies. They reduce mortality and improve cardiac function. Unlike verapamil, they support long-term outcomes.
ACE Inhibitors and ARBs
These reduce afterload and prevent remodeling. They are essential in systolic heart failure management and are well-tolerated when monitored correctly.
Mineralocorticoid Receptor Antagonists
Spironolactone and eplerenone reduce fluid retention and improve survival. They work well in combination with other standard heart failure medications.
SGLT2 Inhibitors
Originally for diabetes, drugs like dapagliflozin have shown benefits in heart failure with reduced ejection fraction. They are now part of guideline-directed medical therapy.
Ivabradine and Digoxin
These may help control heart rate in select cases. They are better tolerated than verapamil in patients with low ejection fraction.
The Role of Cosmetic and Non-Cardiac Considerations
Cosmetic Dental Procedures and Drug Interactions
Patients using verapamil may also take other medications. Some cosmetic dental procedures require antibiotics or local anesthetics. Verapamil can interact with these, increasing the risk of adverse effects such as bradycardia or hypotension during the procedure.
Gum Disease and Cardiovascular Risk
There is a link between gum disease and heart failure. Inflammation from periodontal disease can worsen cardiac conditions. Proper oral hygiene and dental evaluations are essential.
Gum Inflammation and Medication Side Effects
Some medications, including calcium channel blockers, can cause gingival overgrowth. This may contribute to gum inflammation and complicate oral care in heart failure patients.
Pharmacokinetics and Drug Interactions
Liver Metabolism and Bioavailability
Verapamil is metabolized in the liver by CYP3A4 enzymes. Patients with hepatic dysfunction or multiple medications are at higher risk for adverse effects due to drug accumulation.
Interaction With Digoxin
Verapamil increases serum digoxin levels. In heart failure patients, this can increase the risk of digoxin toxicity, especially when kidney function is impaired.
Interaction With Beta-Blockers
Concurrent use with beta-blockers can amplify bradycardia and AV block. This combination should be avoided or used only under close monitoring.
Conclusion
Verapamil is a powerful calcium channel blocker. However, its negative inotropic and chronotropic effects make it unsuitable for most heart failure patients. It can reduce cardiac output, worsen symptoms, and increase the risk of hospitalization.
In patients with systolic heart failure, the risks far outweigh the benefits. Even in diastolic dysfunction, safer alternatives exist. Current guidelines strongly discourage its use unless under exceptional circumstances with proper supervision.
For heart failure management, therapies with proven benefits—like beta-blockers, ACE inhibitors, and SGLT2 inhibitors—should be prioritized. Healthcare providers must consider each patient’s full clinical profile and comorbidities, including dental health, when prescribing medications.
Related topics: