Inferior myocardial infarction (MI) is a heart attack that affects the lower part of the heart, specifically the inferior wall of the left ventricle. This area is usually supplied by the right coronary artery. An inferior MI occurs when blood flow to this region is blocked, causing damage to the heart muscle. Prompt and effective treatment is critical to restore blood flow, limit heart damage, and improve survival.
Understanding Inferior Myocardial Infarction
What Causes Inferior MI?
The main cause of inferior MI is a blockage in the coronary arteries. Most often, this blockage is due to a blood clot forming on a ruptured atherosclerotic plaque. The clot blocks blood flow, leading to oxygen deprivation and damage to the heart muscle.
Symptoms of Inferior MI
Common symptoms include:
- Chest pain or discomfort, often described as pressure or tightness
- Pain that radiates to the jaw, neck, or left arm
- Shortness of breath
- Nausea or vomiting
- Cold sweat
- Dizziness or lightheadedness
Inferior MI may also cause specific signs such as bradycardia (slow heart rate) or hypotension (low blood pressure) due to involvement of the right coronary artery which supplies the sinoatrial (SA) and atrioventricular (AV) nodes.
Initial Emergency Management
Rapid Assessment and Diagnosis
Time is critical in treating inferior MI. The first step is to quickly assess the patient’s symptoms and perform diagnostic tests, including:
- Electrocardiogram (ECG): To identify ST-segment elevation in inferior leads (II, III, aVF)
- Blood tests: Troponin and other cardiac enzymes confirm heart muscle injury
- Physical examination: Check vital signs, heart sounds, and signs of heart failure
Immediate Actions
Once diagnosed or strongly suspected, treatment should start immediately:
- Oxygen therapy: Administer if oxygen saturation is below 90%
- Aspirin: Given immediately to reduce clot formation
- Nitroglycerin: Used to relieve chest pain unless contraindicated by low blood pressure
- Pain relief: Morphine may be used carefully if pain persists
Reperfusion Therapy
Why Reperfusion Is Important
The main goal of treating inferior MI is to restore blood flow to the affected area. This limits heart muscle damage and improves survival. Reperfusion can be done by two main methods:
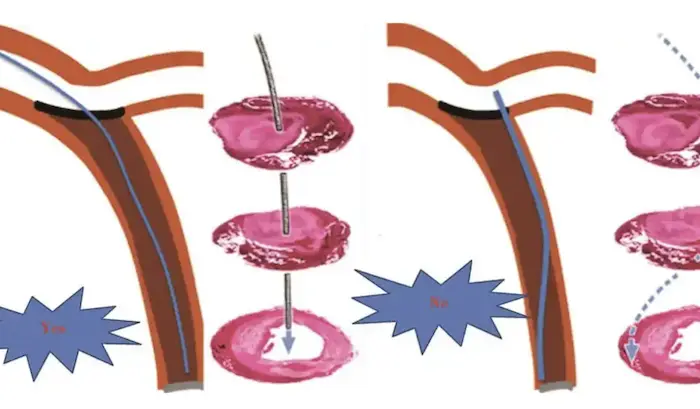
Primary Percutaneous Coronary Intervention (PCI)
PCI is the preferred method when available. It involves threading a catheter through blood vessels to the blocked artery and opening it with a balloon (angioplasty). A stent is usually placed to keep the artery open. PCI offers better outcomes if done quickly, ideally within 90 minutes of hospital arrival.
Thrombolytic Therapy
When PCI is not available within the recommended time, thrombolytic (clot-busting) drugs are used. These medicines dissolve the clot blocking the artery. They are most effective when given within 12 hours of symptom onset. Common thrombolytics include alteplase, reteplase, and tenecteplase.
Medical Management After Reperfusion
Antiplatelet and Anticoagulant Therapy
Medications to prevent new clots and keep arteries open include:
- Aspirin: Continued long-term to reduce clot risk
- P2Y12 inhibitors: Such as clopidogrel, ticagrelor, or prasugrel, used alongside aspirin
- Anticoagulants: Heparin or low molecular weight heparin during hospital stay
Beta-Blockers
Beta-blockers reduce heart rate and oxygen demand. They improve survival if given early, unless contraindicated by low blood pressure or heart failure.
ACE Inhibitors and ARBs
Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) help reduce heart remodeling and heart failure risk after MI.
Statins
Cholesterol-lowering statins are started early to stabilize plaques and reduce future heart attack risk.
Management of Complications
Bradyarrhythmias and Heart Block
Inferior MI can cause slow heart rhythms or blockages in the electrical system due to right coronary artery involvement. Treatment may require temporary pacing to maintain adequate heart rate.
Right Ventricular Infarction
Inferior MI sometimes affects the right ventricle, leading to low blood pressure and poor circulation. Treatment includes careful fluid management and avoiding medications that lower blood pressure further.
Heart Failure
If heart muscle damage is extensive, heart failure can develop. Treatment involves diuretics to reduce fluid overload, and other heart failure medications.
Mechanical Complications
Rare but serious complications include rupture of the heart muscle or valves. These require urgent surgical intervention.
Long-Term Care and Rehabilitation
Cardiac Rehabilitation
After hospital discharge, cardiac rehabilitation programs help patients recover strength and improve heart health through supervised exercise, education, and counseling.
Lifestyle Modifications
Patients must adopt heart-healthy habits:
- Quit smoking
- Eat a balanced diet low in saturated fats and salt
- Exercise regularly
- Maintain healthy weight
- Manage stress
Ongoing Medical Follow-Up
Regular check-ups with a cardiologist are essential. They monitor heart function, medication effects, and screen for complications.
Prognosis of Inferior Myocardial Infarction
Survival Rates
With timely treatment, survival rates after inferior MI have improved dramatically. Early reperfusion therapy reduces heart damage and complications.
Quality of Life
Many patients resume normal activities and have a good quality of life with proper treatment and lifestyle changes.
Risk of Recurrence
Patients remain at risk for future heart attacks. Secondary prevention with medications and lifestyle changes is critical.
Advances in Treatment
Improved Stent Technology
Newer drug-eluting stents reduce re-blockage risk and improve long-term artery patency.
Personalized Medicine
Genetic and biomarker studies help tailor treatments to individual patient risk profiles.
Emerging Therapies
Research into stem cell therapy and novel drugs aims to regenerate heart tissue and reduce damage after MI.
Conclusion
Inferior myocardial infarction is a serious condition but treatable with prompt and appropriate care. Early reperfusion therapy, combined with medication and lifestyle changes, improves survival and quality of life. Close follow-up and rehabilitation are key to long-term health. Advances in treatment continue to enhance outcomes for patients worldwide.
Related topics: