Inferior myocardial infarction (IMI), a type of heart attack that affects the inferior wall of the heart, is a significant clinical concern in cardiology. This condition arises when blood flow to the inferior part of the heart muscle is obstructed, typically due to a blockage in the right coronary artery (RCA) or one of its branches. While inferior myocardial infarctions can sometimes present with less dramatic symptoms than anterior infarctions, they carry unique risks and complications that can lead to severe outcomes, including heart failure, arrhythmias, and even sudden cardiac death. In this article, we will explore the pathophysiology, clinical presentation, diagnostic methods, treatment options, and long-term implications of inferior myocardial infarction.
Understanding Myocardial Infarction
Definition and Types
Myocardial infarction (MI) occurs when blood supply to a part of the heart is interrupted, leading to the death of heart muscle cells. This interruption is most commonly caused by the rupture of an atherosclerotic plaque and subsequent thrombosis. There are two main types of myocardial infarction:
ST-Elevation Myocardial Infarction (STEMI): This type is characterized by a significant elevation of the ST segment on the electrocardiogram (ECG) and typically indicates a complete occlusion of a coronary artery.
Non-ST-Elevation Myocardial Infarction (NSTEMI): This type does not show significant ST elevation but indicates a partial blockage of a coronary artery, often leading to less extensive myocardial damage.
Inferior myocardial infarctions can be classified as either STEMI or NSTEMI, depending on the ECG findings and the extent of myocardial damage.
Anatomy of the Heart
To understand inferior myocardial infarction, it is essential to recognize the anatomy of the heart and the coronary circulation. The heart has four chambers: the left atrium, left ventricle, right atrium, and right ventricle. The coronary arteries supply blood to the heart muscle, and the right coronary artery typically supplies the inferior wall of the heart.
The inferior wall is supplied by:
Right Coronary Artery (RCA): In most individuals, the RCA supplies the inferior wall of the left ventricle and the right ventricle.
Left Circumflex Artery (LCx): In some patients, particularly those with left dominant coronary circulation, the LCx may also supply parts of the inferior wall.
Pathophysiology of Inferior Myocardial Infarction
Inferior myocardial infarction occurs when there is a significant reduction or cessation of blood flow to the inferior wall of the heart. This can happen due to:
Atherosclerosis: The buildup of plaque in the coronary arteries can narrow them, leading to reduced blood flow.
Thrombosis: A ruptured plaque can lead to the formation of a blood clot that completely occludes the artery.
Coronary Vasospasm: In some cases, temporary spasms of the coronary arteries can lead to reduced blood flow and infarction.
When blood flow is interrupted, the affected myocardial tissue becomes ischemic (lacking oxygen) and can begin to die within minutes. The extent of damage depends on the duration of the ischemia and the presence of collateral circulation.
Clinical Presentation of Inferior Myocardial Infarction
Symptoms
The symptoms of inferior myocardial infarction can vary widely among individuals, and some patients may experience atypical presentations. Common symptoms include:
Chest Pain: Often described as a pressure or squeezing sensation in the chest, although some patients may report pain in the upper abdomen or back.
Shortness of Breath: Difficulty breathing can occur due to reduced cardiac output or pulmonary congestion.
Nausea and Vomiting: These symptoms may be more pronounced in inferior MIs compared to other types of MIs.
Diaphoresis: Excessive sweating is a common symptom associated with myocardial infarction.
Fatigue: Unexplained fatigue or weakness, particularly in women, may be an early sign.
Atypical Presentations
Inferior myocardial infarctions can present with atypical symptoms, especially in women, the elderly, and diabetic patients. These can include:
Epigastric Pain: Patients may mistake heart-related pain for gastrointestinal discomfort.
Back Pain: Discomfort in the back can be a misleading symptom.
Palpitations: Irregular heartbeats or a sensation of a racing heart.
Signs on Physical Examination
During a physical examination, healthcare providers may observe:
Hypotension: Low blood pressure can occur due to reduced cardiac output.
Jugular Venous Distension (JVD): This may indicate right-sided heart failure or fluid overload.
S3 or S4 Heart Sounds: These can indicate heart failure or increased filling pressures.
Complications of Inferior Myocardial Infarction
Inferior myocardial infarction can lead to several serious complications, including:
Heart Failure: Damage to the heart muscle can impair its ability to pump effectively, leading to heart failure.
Arrhythmias: The ischemic tissue can disrupt the heart’s electrical conduction system, leading to arrhythmias such as bradycardia, atrioventricular (AV) block, or ventricular tachycardia.
Cardiogenic Shock: Severe heart failure can lead to cardiogenic shock, a life-threatening condition characterized by inadequate tissue perfusion.
Pericarditis: Inflammation of the pericardium can occur after myocardial infarction, leading to chest pain and other symptoms.
Ventricular Rupture: In rare cases, extensive myocardial damage can lead to rupture of the ventricular wall, resulting in a life-threatening situation.
Diagnostic Evaluation
Electrocardiogram (ECG)
The ECG is a critical tool in diagnosing inferior myocardial infarctions. Key features include:
ST Segment Elevation: In STEMI, there will be ST segment elevation in the inferior leads (II, III, and aVF).
Q Waves: The development of pathological Q waves in the inferior leads can indicate a more extensive infarction.
Reciprocal Changes: ST depression may be observed in the anterior leads (I, aVL) as a reciprocal change.
Cardiac Biomarkers
Cardiac biomarkers are essential for diagnosing myocardial infarction and assessing the extent of myocardial damage. The most commonly used biomarkers include:
Troponin I and T: These proteins are released into the bloodstream when cardiac muscle is damaged. Elevated levels indicate myocardial injury and are sensitive and specific for myocardial infarction.
Creatine Kinase-MB (CK-MB): This enzyme can also indicate myocardial injury, although it is less specific than troponin.
Imaging Studies
Echocardiography: This imaging modality can assess cardiac function and wall motion abnormalities. It can help identify areas of the heart that are not contracting effectively due to ischemia.
Cardiac MRI: In select cases, cardiac MRI can provide detailed information about myocardial viability and the extent of infarction.
Coronary Angiography: This invasive procedure is often performed to visualize the coronary arteries and identify any blockages. It is typically done in the setting of STEMI for immediate intervention.
Treatment of Inferior Myocardial Infarction
Initial Management
The initial management of inferior myocardial infarction focuses on restoring blood flow to the affected area and stabilizing the patient. Key components include:
Aspirin and Antiplatelet Therapy: Aspirin is administered to inhibit platelet aggregation and reduce the risk of further clot formation. Other antiplatelet agents, such as clopidogrel or ticagrelor, may also be used.
Anticoagulation: Heparin or low molecular weight heparin may be used to prevent further clot formation.
Oxygen Therapy: Supplemental oxygen may be provided to improve oxygen delivery to the myocardium, especially if the patient is hypoxic.
Nitrates: Nitrates can help relieve chest pain and improve blood flow by dilating coronary arteries.
Beta-Blockers: These medications can reduce heart rate and myocardial oxygen demand, improving outcomes in patients with myocardial infarction.
Statins: High-intensity statin therapy is recommended to lower cholesterol levels and stabilize atherosclerotic plaques.
Reperfusion Therapy
Reperfusion therapy is critical in the management of STEMI and is aimed at restoring blood flow to the affected area as quickly as possible. The two primary modalities are:
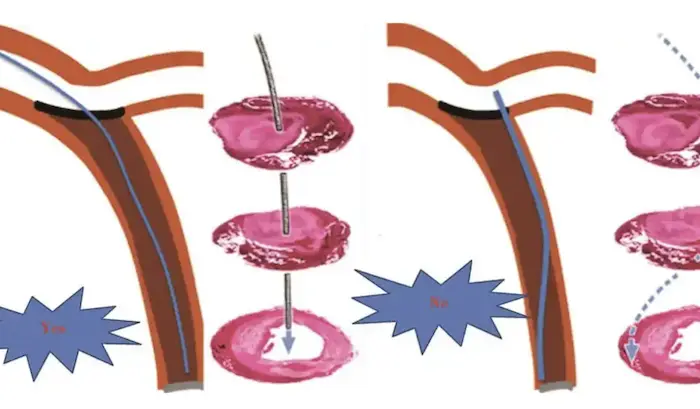
Percutaneous Coronary Intervention (PCI): This minimally invasive procedure involves the insertion of a catheter to open the blocked coronary artery, often accompanied by the placement of a stent to keep the artery open.
Thrombolytic Therapy: In cases where PCI is not immediately available, thrombolytic agents (clot busters) may be administered to dissolve the thrombus and restore blood flow. However, this therapy is less commonly used now due to the effectiveness of PCI.
Management of Complications
Patients with inferior myocardial infarction may require additional management for complications:
Heart Failure: Diuretics, ACE inhibitors, and beta-blockers may be used to manage heart failure symptoms.
Arrhythmias: Antiarrhythmic medications or electrical cardioversion may be necessary for patients with significant arrhythmias.
Cardiogenic Shock: In cases of cardiogenic shock, more aggressive interventions, such as intra-aortic balloon pump (IABP) support or mechanical circulatory support, may be required.
Pericarditis: Nonsteroidal anti-inflammatory drugs (NSAIDs) or colchicine may be used to manage post-MI pericarditis.
Long-Term Management and Prognosis
Lifestyle Modifications
Long-term management of patients with inferior myocardial infarction focuses on preventing recurrence and optimizing cardiovascular health. Key lifestyle modifications include:
Smoking Cessation: Quitting smoking is one of the most effective ways to reduce cardiovascular risk.
Dietary Changes: A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can help lower cholesterol and blood pressure.
Regular Exercise: Engaging in regular physical activity is essential for cardiac rehabilitation and overall health.
Weight Management: Maintaining a healthy weight can reduce the risk of cardiovascular disease.
Medication Adherence
Patients should be encouraged to adhere to prescribed medications, including:
Antiplatelet Agents: Continued use of aspirin and other antiplatelet medications is crucial to prevent future events.
Statins: Statin therapy should be maintained to manage cholesterol levels and reduce cardiovascular risk.
ACE Inhibitors and Beta-Blockers: These medications can help manage heart failure symptoms and reduce the risk of future heart attacks.
Regular Follow-Up
Regular follow-up appointments with healthcare providers are essential for monitoring cardiovascular health and adjusting treatment as needed. This may include:
Cardiac Rehabilitation: Participation in a structured cardiac rehabilitation program can improve outcomes and quality of life.
Monitoring for Complications: Regular assessments for heart failure, arrhythmias, and other complications should be performed.
Psychosocial Support: Addressing the psychological impact of myocardial infarction is vital for long-term recovery.
Conclusion
Inferior myocardial infarction is a critical concern due to its potential to cause significant morbidity and mortality. Understanding the unique aspects of IMI, including its pathophysiology, clinical presentation, complications, and management, is essential for healthcare providers. Early recognition and prompt treatment can improve outcomes and reduce the risk of serious complications.
As we continue to advance our understanding of cardiovascular disease and refine treatment strategies, it is crucial to prioritize patient education and lifestyle modifications to prevent future events. By addressing the multifaceted nature of inferior myocardial infarction, we can enhance the quality of care for patients and improve their long-term prognosis.
Related Topics: