Inferior myocardial infarction (IMI) is a type of heart attack that occurs when blood flow to the heart muscle is obstructed, particularly affecting the inferior wall of the heart. This condition is often diagnosed through an electrocardiogram (ECG or EKG), which provides critical information about the electrical activity of the heart and can reveal characteristic changes associated with an inferior myocardial infarction. Understanding the signs, symptoms, causes, and implications of inferior myocardial infarction is crucial for timely diagnosis and effective treatment.
In this article, we will explore the definition of inferior myocardial infarction, its pathophysiology, the role of the ECG in diagnosis, the typical ECG findings associated with IMI, differential diagnoses, treatment options, and long-term implications for patients.
Understanding Myocardial Infarction
Definition of Myocardial Infarction
Myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow to a part of the heart is blocked for an extended period, causing damage to the heart muscle. This blockage is often due to atherosclerosis, where plaque builds up in the coronary arteries, or it can be caused by a blood clot that forms in a narrowed artery.
Types of Myocardial Infarction
Myocardial infarctions are classified based on their location and the extent of damage:
Anterior Myocardial Infarction: Occurs in the front wall of the heart and is often associated with the left anterior descending artery (LAD).
Inferior Myocardial Infarction: Affects the inferior wall of the heart, typically linked to the right coronary artery (RCA) in right-dominant coronary systems.
Lateral Myocardial Infarction: Involves the side wall of the heart and is often associated with the left circumflex artery (LCX).
Posterior Myocardial Infarction: Involves the back wall of the heart and is less commonly diagnosed.
Pathophysiology of Inferior Myocardial Infarction
Inferior myocardial infarction primarily occurs due to occlusion of the right coronary artery (RCA) or, in some cases, the left circumflex artery (LCX). The RCA supplies blood to the inferior wall of the left ventricle, as well as the right ventricle and the inferior portion of the interventricular septum. When blood flow is interrupted, the affected heart muscle becomes ischemic (lacking oxygen) and can begin to die if blood flow is not restored quickly.
Risk Factors
Several risk factors contribute to the development of myocardial infarction, including:
Coronary Artery Disease (CAD): The most common cause of MI, characterized by the buildup of plaque in the coronary arteries.
Hypertension: High blood pressure can damage arteries and contribute to atherosclerosis.
Diabetes: Diabetes increases the risk of coronary artery disease and myocardial infarction.
Smoking: Tobacco use is a significant risk factor for heart disease.
Obesity: Excess body weight is associated with increased risk factors for heart disease.
Sedentary Lifestyle: Lack of physical activity can contribute to obesity and other risk factors.
Family History: A family history of heart disease can increase an individual’s risk.
The Role of ECG in Diagnosing Inferior Myocardial Infarction
What is an ECG?
An electrocardiogram (ECG) is a non-invasive test that records the electrical activity of the heart over a period of time. It provides valuable information about the heart’s rhythm, the size and position of the heart chambers, and any areas of ischemia or infarction.
Importance of ECG in Myocardial Infarction
The ECG is a critical tool for diagnosing myocardial infarction, as it can reveal characteristic changes that indicate the presence of ischemia or damage to the heart muscle. In the case of inferior myocardial infarction, specific ECG changes can help healthcare providers identify the location and extent of the infarction.
ECG Findings in Inferior Myocardial Infarction
ST-Segment Elevation
One of the hallmark signs of an inferior myocardial infarction is ST-segment elevation in the ECG. This elevation typically occurs in the inferior leads, which are:
- Lead II
- Lead III
- Lead aVF
Reciprocal Changes
In addition to ST-segment elevation in the inferior leads, reciprocal changes may be observed in the anterior leads, particularly:
- Lead I
- Lead aVL
These reciprocal changes can manifest as ST-segment depression in the anterior leads, indicating that the heart muscle is experiencing ischemia.
Q Waves
In some cases of inferior myocardial infarction, pathological Q waves may develop in the inferior leads (II, III, aVF) as a result of necrosis (death of heart muscle tissue). The presence of Q waves indicates that the infarction is no longer acute and may suggest a previous myocardial infarction.
T-Wave Changes
T-wave changes may also be present in inferior myocardial infarction. These changes can include:
T-wave inversion: This may occur in the inferior leads following the acute phase of the infarction.
Other ECG Findings
In addition to the changes mentioned above, other findings may include:
Sinus bradycardia: This may occur due to increased vagal tone, which is common in inferior MIs.
Atrioventricular (AV) block: Inferior MIs can sometimes lead to AV block, particularly if the RCA is occluded and affects the AV node.
Differential Diagnosis of Inferior Myocardial Infarction
While the ECG findings can be indicative of an inferior myocardial infarction, it is essential to consider other conditions that may present similarly. Differential diagnoses include:
Other Types of Myocardial Infarction
Anterior Myocardial Infarction: May show ST-segment elevation in leads V1-V4.
Lateral Myocardial Infarction: ST-segment elevation in leads I, aVL, V5, and V6.
Pericarditis
Acute pericarditis can cause ST-segment elevation across multiple leads, but it is typically associated with a different pattern of T-wave changes and does not usually produce reciprocal changes.
Pulmonary Embolism
Pulmonary embolism may present with ST-segment changes, but it often includes other findings such as right heart strain on the ECG.
Aortic Dissection
Aortic dissection may cause chest pain and ECG changes, but it typically presents with different patterns of ST-segment changes.
Electrolyte Imbalances
Conditions such as hyperkalemia can cause changes in the ECG that may mimic myocardial infarction.
Treatment of Inferior Myocardial Infarction
Immediate Management
The immediate management of inferior myocardial infarction focuses on restoring blood flow to the affected area of the heart. This may include:
Aspirin: Administering aspirin to reduce platelet aggregation and prevent further clot formation.
Anticoagulants: Medications such as heparin may be given to prevent further clotting.
Thrombolytics: In some cases, thrombolytic therapy may be used to dissolve the blood clot obstructing the coronary artery.
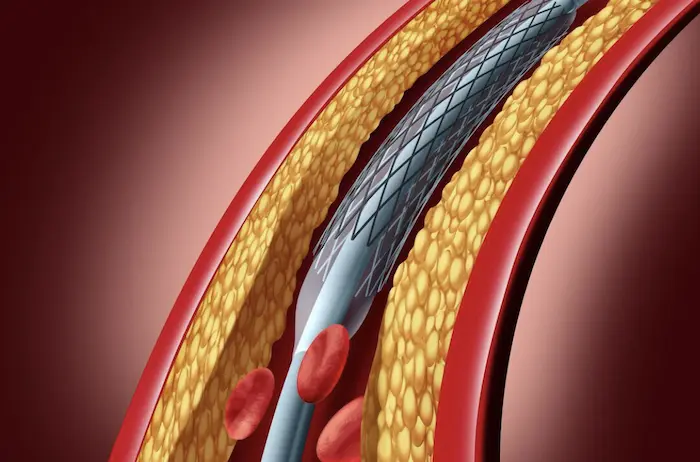
Percutaneous Coronary Intervention (PCI): This procedure involves the use of a catheter to open the blocked artery, often with the placement of a stent to keep the artery open.
Medications
Following the initial management, several medications may be prescribed to help manage the patient’s condition and prevent future events:
Beta-Blockers: These medications can reduce heart rate and myocardial oxygen demand.
ACE Inhibitors: Used to lower blood pressure and reduce strain on the heart.
Statins: Cholesterol-lowering medications that help stabilize plaque and reduce the risk of future cardiovascular events.
Antiplatelet Agents: Medications such as clopidogrel may be prescribed in addition to aspirin to further reduce the risk of clot formation.
Lifestyle Modifications
Patients recovering from an inferior myocardial infarction should be encouraged to adopt heart-healthy lifestyle changes, including:
Diet: Following a heart-healthy diet low in saturated fats, cholesterol, and sodium.
Exercise: Engaging in regular physical activity as advised by a healthcare provider.
Smoking Cessation: Quitting smoking to reduce the risk of future cardiovascular events.
Weight Management: Maintaining a healthy weight to reduce strain on the heart.
Cardiac Rehabilitation
Cardiac rehabilitation is a structured program that helps patients recover from a heart attack, improve their cardiovascular health, and reduce the risk of future heart problems. It typically includes:
Supervised Exercise Training: Gradual increase in physical activity under medical supervision.
Education: Information on heart-healthy living, including diet and stress management.
Psychosocial Support: Counseling and support to help patients cope with the emotional aspects of recovery.
Long-Term Implications of Inferior Myocardial Infarction
Prognosis
The prognosis for patients with inferior myocardial infarction varies depending on several factors, including the extent of damage to the heart muscle, the presence of comorbidities, and the timeliness of treatment. With prompt and appropriate management, many patients can recover well and return to normal activities.
Risk of Future Events
Patients who have experienced a myocardial infarction are at increased risk for future cardiovascular events, including recurrent myocardial infarction, heart failure, and arrhythmias. Ongoing management, lifestyle changes, and adherence to medication regimens are crucial for reducing this risk.
Psychological Impact
Experiencing a myocardial infarction can have significant psychological effects, including anxiety and depression. It is important for healthcare providers to address these concerns and offer support as needed.
Regular Follow-Up Care
Patients who have had an inferior myocardial infarction should have regular follow-up appointments with their healthcare providers to monitor their heart health, adjust medications as needed, and assess for any ongoing symptoms.
Conclusion
Inferior myocardial infarction is a serious condition that requires prompt recognition and treatment. The electrocardiogram plays a vital role in diagnosing this condition, with characteristic findings such as ST-segment elevation in the inferior leads and reciprocal changes in the anterior leads. Understanding the signs, symptoms, and implications of inferior myocardial infarction is essential for effective management and improving patient outcomes.
With timely intervention and appropriate follow-up care, many individuals can recover from an inferior myocardial infarction and lead healthy, active lives. It is crucial for patients to be aware of their risk factors, adhere to treatment plans, and engage in heart-healthy lifestyle changes to minimize the risk of future cardiovascular events.
Related Topics: