Tachycardia is a cardiac condition characterized by an abnormally fast heart rate, typically defined as a resting heart rate exceeding 100 beats per minute. It can range from a benign physiological response to a potentially life-threatening arrhythmia, depending on its type and underlying cause. Understanding the symptoms, causes, and treatment options is crucial for effective management and prevention of complications.
What Is Tachycardia?
Tachycardia refers to an elevated heart rate that originates from abnormal electrical activity in the heart. The heart normally beats between 60 and 100 times per minute at rest. When the rate exceeds 100 beats per minute, it is classified as tachycardia. There are several types, including:
Sinus tachycardia: A faster-than-normal heart rate originating from the sinus node, the heart’s natural pacemaker.
Supraventricular tachycardia (SVT): Rapid heartbeats originating above the ventricles, often due to abnormal electrical pathways.
Ventricular tachycardia (VT): Fast heart rate starting in the ventricles, which can be life-threatening.
Each type has distinct causes, symptoms, and treatment approaches.
Causes of Tachycardia
Tachycardia can be triggered by a variety of physiological, pathological, and external factors. These causes can be broadly categorized into:
1. Physiological and External Causes
Exercise and physical activity: Increased oxygen demand causes the heart to beat faster.
Emotional stress, anxiety, fear: Release of adrenaline stimulates the heart rate.
Fever and infections: Increase metabolic demand and heart rate.
Stimulants: Caffeine, tobacco, certain medications, and illegal drugs such as cocaine and methamphetamine can provoke tachycardia.
Medications: Some drugs, including decongestants and thyroid medications, can increase heart rate.
2. Medical and Cardiac Causes
Heart conditions: High blood pressure, heart failure, myocarditis (heart infection), coronary artery disease, and structural heart disease.
Arrhythmias: Abnormal electrical pathways cause irregular rapid heart rhythms, such as atrial fibrillation or ventricular tachycardia.
Thyroid disorders: Hyperthyroidism accelerates metabolism and heart rate.
Anemia: Low red blood cell count reduces oxygen delivery, causing compensatory tachycardia.
Electrolyte imbalances: Abnormal potassium, calcium, sodium, or magnesium levels disrupt electrical conduction.
Sleep apnea and obesity: Conditions that strain the heart and increase risk.
Congenital abnormalities: Extra electrical pathways or inherited syndromes like long QT syndrome.
In some cases, the exact cause remains unknown.
Symptoms of Tachycardia
Symptoms vary depending on the type and severity of tachycardia. Some individuals may be asymptomatic, especially if the tachycardia is mild or transient. When symptoms occur, they commonly include:
- Palpitations: Sensation of rapid, fluttering, or pounding heartbeats.
- Dizziness or lightheadedness
- Shortness of breath
- Chest pain or discomfort
- Fainting or syncope
- Weakness or fatigue
- Anxiety or a feeling of impending doom
- Cold sweats
In severe cases, especially with ventricular tachycardia, symptoms can escalate to cardiac arrest if untreated.
Diagnosis of Tachycardia
Diagnosis involves a thorough clinical evaluation including:
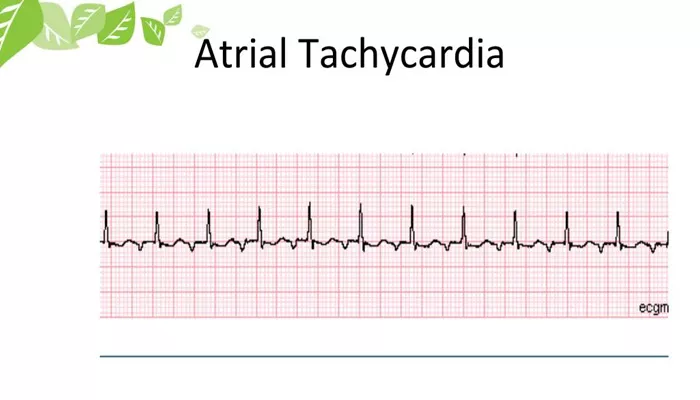
Electrocardiogram (ECG/EKG): To identify the type of tachycardia and its origin.
Holter monitor or event recorder: For intermittent symptoms.
Blood tests: To check for anemia, thyroid function, and electrolyte levels.
Echocardiogram: To assess structural heart disease.
Stress testing and electrophysiological studies: In selected cases to pinpoint arrhythmia sources.
Treatment of Tachycardia
Treatment depends on the tachycardia type, symptoms, underlying cause, and risk of complications.
1. Lifestyle Modifications
Avoid stimulants such as caffeine, tobacco, and illicit drugs.
Manage stress through relaxation techniques.
Maintain a heart-healthy diet and regular exercise.
Control underlying conditions like hypertension, thyroid disease, and anemia.
2. Medications
Rate control agents: Beta-blockers (e.g., atenolol, metoprolol), calcium channel blockers (e.g., diltiazem, verapamil), and digitalis slow the heart rate.
Antiarrhythmic drugs: Amiodarone, propafenone, and sotalol help maintain normal rhythm.
Anticoagulants: Aspirin or warfarin reduce stroke risk in atrial arrhythmias.
3. Non-surgical Procedures
Cardioversion: Electrical shock to restore normal rhythm in emergencies or persistent arrhythmias.
Catheter ablation: A minimally invasive procedure that destroys abnormal electrical pathways causing tachycardia, often curative for supraventricular and some ventricular tachycardias.
Stereotactic body radiation therapy (SBRT): Experimental for refractory ventricular tachycardia.
4. Surgical and Device Therapies
Implantable cardioverter-defibrillator (ICD): Monitors heart rhythm and delivers shocks to correct life-threatening arrhythmias.
Pacemaker implantation: For bradycardia or to regulate heart rhythm.
Maze procedure: Surgical intervention for atrial fibrillation involving scar creation to block abnormal signals.
Left atrial appendage occlusion: Reduces stroke risk in atrial fibrillation patients.
Complications of Untreated Tachycardia
If left unmanaged, tachycardia can lead to:
Inadequate cardiac output causing organ hypoxia.
Blood clots leading to stroke or heart attack.
Heart failure due to sustained rapid heart rate.
Sudden cardiac death, particularly with ventricular tachycardia or fibrillation.
Conclusion
Tachycardia is a common cardiac condition with diverse causes ranging from benign physiological responses to serious cardiac disorders. Recognizing symptoms and seeking timely medical evaluation is essential. Advances in diagnostic techniques and treatments, including medications, catheter ablation, and implantable devices, have significantly improved outcomes. A multidisciplinary approach tailored to the individual patient’s condition and lifestyle is key to effective management and prevention of complications.
Related topics: