Junctional bradycardia is a type of arrhythmia, characterized by a slow heart rate originating from the junctional area of the heart, which is located between the atria and the ventricles. Unlike the normal sinus rhythm, where the sinoatrial (SA) node controls the heart rate, junctional bradycardia occurs when the heart’s electrical impulses are generated from the atrioventricular (AV) junction or nearby tissues.
This condition can lead to a heart rate of fewer than 60 beats per minute, and in some cases, it may cause symptoms such as fatigue, dizziness, and fainting. Junctional bradycardia can be transient or persistent, and its severity often depends on its underlying cause. While it is often benign, it can sometimes indicate a more serious underlying issue.
In this article, we will explore the symptoms, causes, and treatment options for junctional bradycardia. We will also discuss how this condition is diagnosed and the potential complications that may arise if left untreated.
What is Junctional Bradycardia?
Junctional bradycardia occurs when the electrical impulses that control the heart’s rhythm originate from the AV junction instead of the normal SA node. The AV junction can generate electrical signals, but these signals are typically slower than those generated by the SA node, leading to a slower heart rate.
This type of bradycardia is typically classified as a form of “escape rhythm,” meaning that the AV junction takes over pacing the heart when the SA node fails to do so. This condition may arise due to various factors, such as sinus node dysfunction, medications, or underlying heart disease.
What Are the Main Causes of Junctional Bradycardia?
Junctional bradycardia can occur due to various factors, including intrinsic heart conditions, medication use, or disturbances in the electrical conduction system of the heart. Here are the most common causes:
1. Sinus Node Dysfunction
Sinus node dysfunction, or sick sinus syndrome, is one of the primary causes of junctional bradycardia. When the SA node is not functioning properly, the AV junction may take over as the pacemaker of the heart, leading to a slower heart rate. This condition is more common in older adults.
2. Medications
Certain medications can slow the heart rate and contribute to junctional bradycardia. Common drugs that may cause this condition include:
Beta-blockers: Used to treat high blood pressure, arrhythmias, and other cardiovascular conditions.
Calcium channel blockers: These drugs are used for treating hypertension and certain types of arrhythmias.
Digoxin: A medication that increases the strength of the heart’s contractions but can also slow the heart rate.
These medications may alter the electrical activity of the heart and lead to a slower rhythm, sometimes resulting in junctional bradycardia.
3. Heart Disease
Underlying heart diseases, such as coronary artery disease, heart failure, or myocarditis, can also contribute to the development of junctional bradycardia. These conditions can damage the heart’s electrical conduction system, leading to irregular or slow heart rhythms.
4. Electrolyte Imbalances
Imbalances in the body’s electrolytes, such as potassium, calcium, and magnesium, can affect the electrical conduction of the heart and contribute to junctional bradycardia. These imbalances can occur due to dehydration, kidney problems, or certain medications.
5. Acute Myocardial Infarction (Heart Attack)
During or after a heart attack, the heart’s electrical system can become disrupted, potentially leading to junctional bradycardia. This may be a temporary condition as the heart heals, but in some cases, it can become chronic.
6. Hypothyroidism
An underactive thyroid (hypothyroidism) can slow the metabolism and lead to bradycardia, including junctional bradycardia. Thyroid hormones are essential for the regulation of heart rate, and when their levels are low, the heart rate may decrease.
7. Idiopathic Causes
In some cases, no underlying cause of junctional bradycardia can be identified, and the condition is considered idiopathic. These cases may not cause significant symptoms and may not require treatment unless complications arise.
Symptoms of Junctional Bradycardia
The symptoms of junctional bradycardia can vary depending on the severity of the condition and whether it is associated with any other cardiovascular issues. Some individuals with junctional bradycardia may not experience any symptoms at all, while others may have symptoms that significantly impact their quality of life.
Common Symptoms
Fatigue: A common symptom of junctional bradycardia, as a slower heart rate can result in reduced blood flow and less oxygen delivery to tissues.
Dizziness or Lightheadedness: Reduced blood flow to the brain can cause these symptoms, especially when standing up quickly.
Fainting (Syncope): In more severe cases, a drop in heart rate may result in fainting, as the body does not receive adequate blood flow.
Shortness of Breath: Some individuals may experience difficulty breathing, particularly during physical activity or exertion.
Chest Pain: Although less common, chest discomfort can occur if the heart is not pumping efficiently.
Serious Symptoms and Complications
In rare cases, junctional bradycardia can lead to more severe symptoms, such as:
Heart failure: If the heart is unable to pump blood effectively due to the slow heart rate, heart failure symptoms such as swelling in the legs or ankles may develop.
Shock: Severe and prolonged bradycardia can lead to circulatory shock, where the body’s vital organs are not receiving enough blood and oxygen.
Diagnosis of Junctional Bradycardia
The diagnosis of junctional bradycardia typically involves several diagnostic tools and tests to identify the underlying cause and assess the severity of the condition.
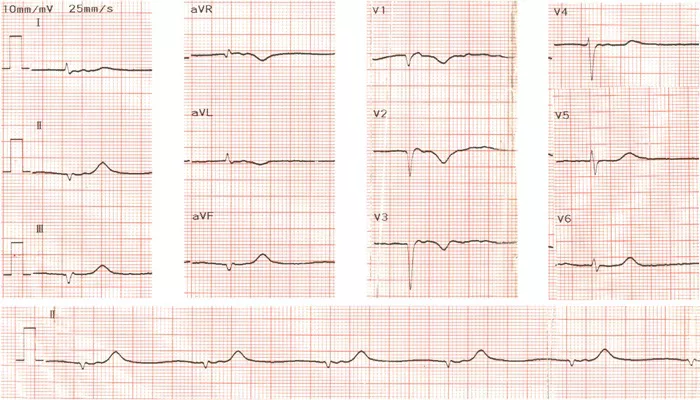
1. Electrocardiogram (ECG)
An electrocardiogram (ECG or EKG) is the primary diagnostic tool used to diagnose junctional bradycardia. It provides a visual representation of the electrical activity of the heart and can confirm the presence of a slow heart rate originating from the AV junction.
On an ECG, junctional bradycardia is typically characterized by:
P waves that are absent, inverted, or delayed.
A slower than normal heart rate (less than 60 beats per minute).
A narrow QRS complex.
2. Holter Monitoring
A Holter monitor is a portable ECG device that records the heart’s electrical activity over 24 to 48 hours. This test is useful for detecting intermittent junctional bradycardia or identifying patterns in heart rate fluctuations throughout the day.
3. Blood Tests
Blood tests can help assess electrolyte levels, thyroid function, and other markers that may contribute to junctional bradycardia. Abnormal results may guide further treatment or indicate the need for additional tests.
4. Echocardiogram
An echocardiogram is an ultrasound of the heart that provides detailed images of the heart’s structure and function. It can help identify any underlying heart conditions, such as heart disease or heart valve issues, that may contribute to junctional bradycardia.
Treatment of Junctional Bradycardia
The treatment of junctional bradycardia depends on the underlying cause and the severity of the symptoms. In some cases, no treatment may be required if the condition is asymptomatic or mild. However, if junctional bradycardia leads to symptoms or complications, treatment options may include:
1. Medication Adjustment
If medications are causing junctional bradycardia, adjusting the dosage or switching to an alternative medication may help alleviate symptoms. For example, reducing or discontinuing beta-blockers or calcium channel blockers may improve heart rate.
2. Pacemaker Implantation
In cases where junctional bradycardia is symptomatic and persistent, or when it results in fainting or other complications, a pacemaker may be recommended. A pacemaker is a small device implanted under the skin that helps regulate the heart’s rhythm by sending electrical impulses to the heart when necessary.
3. Treatment of Underlying Conditions
If an underlying condition, such as heart disease, hypothyroidism, or an electrolyte imbalance, is contributing to junctional bradycardia, treating the condition may help resolve the bradycardia. For example, thyroid hormone replacement for hypothyroidism or correction of electrolyte imbalances can improve heart rate.
4. Observation and Lifestyle Modifications
In cases where junctional bradycardia is asymptomatic and not causing any complications, the patient may simply be monitored over time. Lifestyle modifications, such as maintaining a healthy diet, exercising regularly, and avoiding stress, can also help manage heart health and improve symptoms.
Conclusion
Junctional bradycardia is a condition where the heart rate is slower than normal due to abnormal electrical impulses originating from the AV junction. While it is often benign, it can cause symptoms such as fatigue, dizziness, and fainting, especially if it is related to an underlying heart condition or medication use. The treatment of junctional bradycardia depends on the severity of the symptoms and the underlying cause, and in many cases, a pacemaker may be necessary for management.
Related topics: