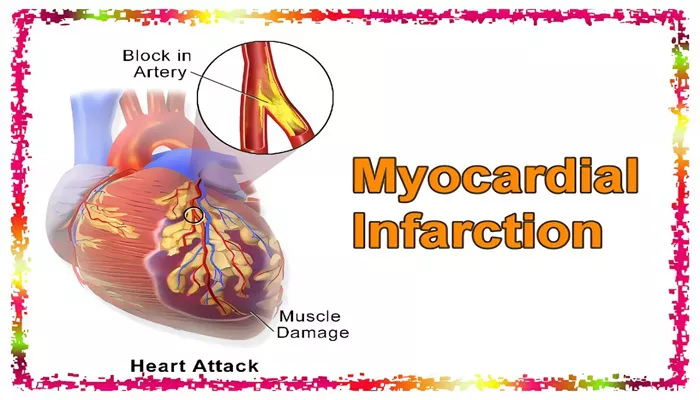
Acute inferior myocardial infarction (IMI) refers to a heart attack that affects the inferior wall of the heart, primarily supplied by the right coronary artery (RCA). Myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow to a part of the heart muscle is blocked, resulting in tissue damage. Acute inferior MI specifically involves the damage to the heart’s lower part, which is crucial for proper cardiac function. Understanding the mechanisms, symptoms, and treatment options for this condition is vital for both patients and healthcare professionals.
What is Acute Inferior Myocardial Infarction?
Definition and Mechanism
Acute inferior myocardial infarction (IMI) is a type of heart attack that occurs when there is a blockage in the blood vessels that supply the inferior (bottom) part of the heart muscle. This blockage typically affects the right coronary artery (RCA), although it can sometimes involve other coronary arteries or their branches. The blockage prevents oxygen-rich blood from reaching the heart muscle, causing ischemia (lack of oxygen), followed by tissue death if not treated promptly. As a result, the heart’s ability to pump blood efficiently is compromised.
Causes of Acute Inferior Myocardial Infarction
The primary cause of acute inferior myocardial infarction is a blockage in one of the coronary arteries due to atherosclerosis (the buildup of fatty deposits or plaques in the arteries). The rupture of a plaque, along with the formation of a blood clot, can obstruct the artery and lead to an acute MI. Other factors contributing to acute inferior MI include:
Coronary artery spasm: Temporary narrowing or constriction of the artery.
Embolism: A clot or other debris traveling from another part of the body and blocking the artery.
Aortic dissection: A tear in the aorta leading to compromised blood flow.
Symptoms of Acute Inferior Myocardial Infarction
Chest Pain
The most common symptom of acute inferior myocardial infarction is chest pain, which may radiate to the left arm, jaw, neck, or back. The pain is typically described as a heavy, squeezing, or pressure-like sensation. It can vary in intensity and duration, often worsening with physical exertion or stress.
Shortness of Breath
Patients experiencing acute inferior MI may also feel shortness of breath due to the impaired pumping function of the heart. The inability of the heart to pump effectively can lead to fluid accumulation in the lungs (pulmonary edema), causing difficulty breathing.
Other Symptoms
Other symptoms may include:
Nausea or vomiting: These symptoms can occur, especially in individuals with lower chest pain or atypical presentations.
Fatigue: Severe fatigue may develop as a result of reduced cardiac output.
Lightheadedness or dizziness: This may occur due to a drop in blood pressure.
Cold sweats: A sign of shock or severe distress in the body.
Diagnosis of Acute Inferior Myocardial Infarction
Electrocardiogram (ECG)
The electrocardiogram (ECG) is a key diagnostic tool for detecting acute inferior myocardial infarction. In this condition, the ECG typically shows ST-segment elevation in the inferior leads (II, III, and aVF). This finding indicates that a significant portion of the heart’s inferior wall is deprived of oxygen due to the blockage of blood flow.
Cardiac Biomarkers
Blood tests for cardiac biomarkers, such as troponin and creatine kinase-MB (CK-MB), are commonly used to confirm the diagnosis. Elevated levels of these proteins indicate that heart muscle tissue has been damaged, helping doctors assess the severity of the infarction.
Coronary Angiography
Coronary angiography is often performed to identify the location and extent of the blockage. During this procedure, a contrast dye is injected into the coronary arteries, and X-ray images are taken to visualize the blood flow. This allows physicians to pinpoint the obstruction and plan appropriate interventions.
Treatment of Acute Inferior Myocardial Infarction
Initial Medical Management
Initial treatment for acute inferior myocardial infarction aims to restore blood flow to the affected part of the heart. The following interventions are commonly used in the emergency department:
Aspirin: Administered to inhibit platelet aggregation and prevent the formation of new clots.
Anticoagulants: Medications like heparin are given to prevent further clot formation.
Thrombolytics: In some cases, clot-busting medications are administered to dissolve the blockage and restore blood flow to the heart.
Beta-blockers: These drugs reduce the heart’s workload by slowing the heart rate and lowering blood pressure, which helps minimize damage to the heart.
Nitrates: Nitrates are used to relieve chest pain and reduce the heart’s oxygen demand.
Percutaneous Coronary Intervention (PCI)
Percutaneous coronary intervention, also known as coronary angioplasty, is often performed to open the blocked artery. A balloon catheter is inserted through a blood vessel and inflated at the site of the blockage, restoring blood flow. In many cases, a stent (a small mesh tube) is placed to keep the artery open and prevent re-blockage.
Coronary Artery Bypass Grafting (CABG)
In more severe cases of acute inferior myocardial infarction or when PCI is not possible, coronary artery bypass grafting (CABG) may be required. This surgical procedure involves taking a healthy blood vessel from another part of the body and grafting it to the blocked coronary artery to bypass the obstruction and restore blood flow to the heart.
Complications of Acute Inferior Myocardial Infarction
Arrhythmias
One of the major complications of acute inferior myocardial infarction is arrhythmias (irregular heart rhythms). These can occur due to the disruption of the heart’s electrical system caused by the infarction. Common arrhythmias include atrial fibrillation, ventricular tachycardia, and ventricular fibrillation, all of which can be life-threatening.
Heart Failure
If a significant portion of the heart muscle is damaged, acute inferior myocardial infarction can lead to heart failure. This condition occurs when the heart is no longer able to pump blood efficiently, leading to fluid buildup in the lungs and other parts of the body.
Cardiogenic Shock
Cardiogenic shock is a severe complication in which the heart fails to pump sufficient blood to meet the body’s needs. It often occurs when a large area of the heart muscle is damaged and can be fatal if not treated promptly.
Prevention and Risk Factor Management
Control of Blood Pressure and Cholesterol
Managing risk factors, such as high blood pressure and high cholesterol, is essential in preventing acute inferior myocardial infarction. Regular monitoring of these parameters can help detect and manage early signs of cardiovascular disease.
Smoking Cessation
Smoking is a major risk factor for the development of atherosclerosis and coronary artery disease. Quitting smoking can significantly reduce the risk of myocardial infarction and other cardiovascular events.
Physical Activity and Diet
Regular physical activity and a heart-healthy diet are crucial in preventing cardiovascular diseases, including acute inferior myocardial infarction. A diet low in saturated fats, cholesterol, and sodium, combined with regular exercise, can improve overall heart health and reduce the risk of heart attacks.
Conclusion
Acute inferior myocardial infarction is a serious condition that affects the heart’s ability to function properly, primarily due to a blockage in the right coronary artery. Early diagnosis, timely intervention, and effective management strategies are essential for improving outcomes and minimizing complications. By understanding the causes, symptoms, treatment options, and preventive measures, individuals can better manage their heart health and reduce their risk of acute inferior myocardial infarction. Regular check-ups, lifestyle modifications, and adherence to medical recommendations can play a crucial role in heart attack prevention.
Related topics: