Pericarditis is the inflammation of the pericardium, the protective sac surrounding the heart. This condition can result from various factors, including infections, autoimmune diseases, and trauma. Bradycardia, on the other hand, refers to a slow heart rate, typically defined as fewer than 60 beats per minute in adults. In some cases, pericarditis can lead to bradycardia, which may present a significant risk to the patient’s health if not managed appropriately.
The connection between pericarditis and bradycardia lies in the heart’s electrical system, which can be disrupted by the inflammation of the pericardium. This article delves into the mechanisms by which pericarditis can cause bradycardia, the symptoms, causes, diagnostic approaches, and treatment strategies available for individuals with both conditions.
The Mechanism of Bradycardia in Pericarditis
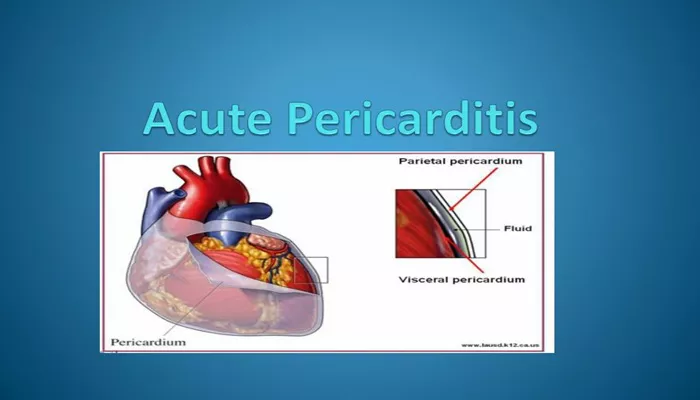
Bradycardia in pericarditis is often related to the electrical disturbances caused by the inflammation of the pericardium. The pericardium, a double-layered membrane, envelops the heart and helps it function smoothly. When the pericardium becomes inflamed, this can lead to interference with the electrical impulses that regulate the heart rate, potentially resulting in bradycardia.
Electrical Conduction Disruption
The heart’s rhythm is controlled by electrical impulses that originate in the sinoatrial (SA) node, the heart’s natural pacemaker. These impulses travel through the atria, the ventricles, and the atrioventricular (AV) node, eventually reaching the ventricles. If the pericardium becomes inflamed, it can cause pressure on the heart’s electrical conduction system, leading to a slower heart rate. The AV node, in particular, may be affected, leading to delayed conduction and bradycardia.
Inflammatory Effects on the AV Node
The AV node is a key component of the heart’s electrical conduction system, acting as a gatekeeper between the atria and the ventricles. Inflammation caused by pericarditis can affect the AV node, reducing the efficiency of electrical signals and leading to a slower heart rate. This is particularly true in cases of pericarditis with significant inflammation, where the pressure exerted on the heart can disrupt normal electrical conduction.
Friction and Pressure on the Heart
Pericarditis can also cause friction between the layers of the pericardium, leading to increased pressure on the heart. This pressure can interfere with the normal rhythm of the heart and contribute to bradycardia. In some cases, pericarditis can lead to a condition known as “constrictive pericarditis,” where the pericardium becomes thickened and stiff, further impacting the electrical conduction of the heart.
Symptoms of Pericarditis and Bradycardia
When pericarditis causes bradycardia, the symptoms can be diverse and may vary based on the severity of both conditions.
It is important to recognize the signs of both pericarditis and bradycardia in order to seek timely medical attention.
Symptoms of Pericarditis
Common symptoms of pericarditis include:
- Sharp or stabbing chest pain, often worse when lying down or breathing deeply
- Difficulty breathing or shortness of breath
- Fever
- Fatigue
- Dry cough
- Swelling in the abdomen or legs
Symptoms of Bradycardia
Bradycardia may cause the following symptoms:
- Dizziness or lightheadedness
- Fatigue or weakness
- Shortness of breath
- Fainting or near-fainting episodes
- Chest pain
- Confusion or memory problems
Symptoms When Both Conditions Coexist
When pericarditis and bradycardia occur together, the symptoms can overlap, and patients may experience a combination of chest pain, dizziness, and shortness of breath. Bradycardia may worsen the symptoms of pericarditis, as reduced blood flow to vital organs can increase fatigue and dizziness.
Causes of Pericarditis and Bradycardia
Pericarditis can result from a wide range of factors, including infections, autoimmune conditions, and trauma. The causes of bradycardia, on the other hand, are often related to issues with the heart’s electrical conduction system. Understanding the causes of both conditions is crucial to effectively managing the risk of bradycardia in patients with pericarditis.
Causes of Pericarditis
Pericarditis can be caused by a variety of factors, including:
Viral Infections: The most common cause of pericarditis is viral infection, such as the coxsackievirus, influenza, or HIV.
Bacterial Infections: Bacterial infections, including tuberculosis and pneumonia, can also lead to pericarditis.
Autoimmune Diseases: Conditions like lupus or rheumatoid arthritis can result in inflammation of the pericardium.
Trauma or Injury: Chest trauma or surgery can lead to inflammation of the pericardium.
Medications: Certain drugs, such as hydralazine or procainamide, can cause drug-induced pericarditis.
Causes of Bradycardia
Bradycardia can result from various factors, including:
Heart Disease: Conditions such as heart attack, heart failure, or heart valve disease can cause bradycardia.
Electrolyte Imbalances: Low levels of potassium or calcium can disrupt the electrical signals in the heart.
Medications: Certain medications, including beta-blockers, calcium channel blockers, and antiarrhythmic drugs, can lower the heart rate.
Vagal Nerve Stimulation: Increased vagal nerve activity can slow the heart rate, often seen in athletes or during sleep.
Pericarditis as a Cause of Bradycardia
Pericarditis may lead to bradycardia through inflammation of the heart’s conduction system, particularly the AV node. The pressure exerted by the inflamed pericardium can affect the electrical signals traveling through the heart, resulting in a slower heart rate. In some cases, pericarditis may cause additional complications such as heart block, further exacerbating bradycardia.
Diagnosis of Pericarditis and Bradycardia
Diagnosing both pericarditis and bradycardia involves a combination of clinical evaluation, diagnostic tests, and imaging studies. Proper diagnosis is essential to determine the underlying causes and initiate appropriate treatment.
Physical Examination
A thorough physical examination is the first step in diagnosing pericarditis and bradycardia. During the examination, the healthcare provider may listen for characteristic heart sounds, such as the pericardial friction rub, which is indicative of pericarditis.
Electrocardiogram (ECG)
An electrocardiogram (ECG) is critical for diagnosing bradycardia. It records the electrical activity of the heart and can help identify abnormal rhythms and conduction issues. In patients with pericarditis, an ECG may show characteristic changes, such as ST-segment elevation, which can help confirm the diagnosis of pericarditis.
Chest X-ray and Echocardiogram
A chest X-ray may help identify signs of pericardial effusion, a condition where fluid accumulates in the pericardium due to inflammation. An echocardiogram provides more detailed images of the heart and can assess its function, looking for evidence of pericardial inflammation or thickening.
Treatment of Pericarditis and Bradycardia
Treatment for pericarditis and bradycardia aims to address both conditions and improve heart function. The approach depends on the severity of each condition, the underlying cause, and the patient’s overall health.
Medications for Pericarditis
The treatment for pericarditis typically involves medications to reduce inflammation and manage pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to alleviate pain and inflammation. In some cases, colchicine or corticosteroids may be prescribed if the inflammation is severe or recurrent.
Medications for Bradycardia
If bradycardia is causing symptoms, medications may be used to speed up the heart rate. Atropine is a common drug used in emergency settings to treat bradycardia by blocking the vagus nerve’s influence on the heart. In some cases, a pacemaker may be needed to regulate the heart rate if the bradycardia is severe or persistent.
Management of Severe Cases
In severe cases of pericarditis or bradycardia, hospitalization may be necessary. If pericarditis leads to complications such as pericardial effusion or constrictive pericarditis, more advanced interventions, such as pericardiocentesis (removal of fluid from the pericardium), may be required.
Conclusion
Pericarditis and bradycardia can occur together, with inflammation of the pericardium potentially leading to disruptions in the heart’s electrical system. Early diagnosis and treatment are crucial in managing both conditions and preventing further complications. With proper care, patients can manage symptoms and reduce the risks associated with pericarditis-induced bradycardia.
Related topics: